Pandemical healthcare architecture and social responsibility — COVID-19 and beyond
White Paper — University of Toronto Centre for Design + Health Innovation
Stephen Verderber, Arch.D., RA, NCARB
ACSA Distinguished Professor
John H. Daniels Faculty of Architecture, Landscape and Design
Director, Centre for Design + Health Innovation
Adjunct Professor, Institute of Health Policy, Management and Evaluation (IHPME)/Dalla Lana School of Public Health
University of Toronto
“Architecture is the reaching out for the truth.”
—Louis Kahn
Executive summary
For centuries, hospitals have been constructed with the primary aim of caring for the ill and to isolate contagious from non-infectious patients. When a medieval or ancient city was stricken by plague, the city would close itself off physically to prevent further contagion by means of fortified walls and gates. The COVID-19 pandemic has cast in sharp relief the intense pressures placed on healthcare facilities to effectively respond to this global public health crisis. Hospital-based intensive care units and long-term-care residential environments for the aged were but two facility types pushed to the limit. In the case of testing, immunization facilities, acute care hospitals, and quarantine housing, the need was great for ancillary, adjunctive facilities capable of being transported to the site of a parking lot or medical centre and set up for the provision of care.
Modular prefabricated pop-up COVID-19 testing and immunization centres were needed. The capacity of architecture to respond effectively to this pandemic is examined below vis-à-vis a review of numerous unbuilt and built projects put forth in 2020—representing a continuum from walk-up testing booths set up on urban sidewalks to the 10,000-bed surge field hospital quickly erected in Wuhan, China. Four types of pandemical facilities are classified: pop-up portable outdoor facilities; pop-up vehicular-nomad facilities; pop-ups installed in repurposed host structures; and 24/7 ICU-based surge capacity field hospitals and quarantine units installed as pop-ups in host structures or as freestanding installations. The recent work of the University of Toronto‘s Architecture + Health graduate design studio is also assessed in the context of this review. This wave of pandemical architecture for health is collectively reviewed in terms of its biophilic and salutogenic content, and its social advocacy and ethical ramifications.
Findings: Many of these walk-up/drive-up and 24/7 surge field hospitals were deemed inadequate in key respects: 1.Lack of patient confidentiality and privacy; 2. Inadequate circulation pathways to separate symptomatic from asymptomatic individuals awaiting testing and/or immunization; 3. Inadequate staff workspaces and insufficient storage for supplies such as PPE equipment, refrigerators, and laboratory equipment; 4. Inadequate protection from the elements for persons using outdoor testing and/or immunization facilities; 5. Windowless conditions in 24/7 facilities that preclude the occupant’s direct contact with natural daylight, views, landscape, or natural ventilation (where appropriate), and inadequate artificial lighting options; 6. Absence of representational (surrogate) nature-themed content and especially in windowless and insufficiently windowed spaces where a mural, actual window, window treatment, and bedside pull curtain would help ameliorate an otherwise under-stimulating, confining physical setting; 7. Monochromatic interior spaces difficult to navigate due to a convoluted spatial layout, worsened by ineffective directional graphics; and 8. Overcrowded patient housing units, resulting in inadequate privacy and confidentiality, compounded by the lack of bedside amenities. Finally, these University-based and external projects are reviewed collectively in terms of their potential contribution to the current discourse in public health-focused public interest architecture. Note to the reader: This review is by no means exhaustive although it is indicative of the international architectural community’s response to this global pandemic.
Key Recommendation: Architects and architectural educators must endeavour to achieve an anticipatory, therapeutic, socially responsive architecture for health in light of current and future uncertainties associated with global climate change, health emergencies, natural and human-induced disasters.
Principal Audiences: Architects, architectural educators and students, engineers, interior designers, evidence-based health and the built environment researchers, administrators of healthcare organizations in the public and private sectors, public health policy specialists, physicians, nurses, and epidemiologists.
Introduction
For centuries, hospitals have been constructed with the primary aim of caring for the ill and to isolate contagious from non-infectious patients. When a medieval or ancient city was stricken by plague, the city would rapidly close itself off physically to prevent further contagion by means of fortified walls and gates. In 17th century Europe, city residents would be confined to their homes and made to appear in their windows during daily inspections to ensure that all were present and accounted for. Small, hastily built wooden canals would lead from residences into a common street for the transportation of rations (and bodies). Imposed lockdowns were common in such dire conditions, and continue to this day as a timeless public health response to disease and plague. During the recent Ebola outbreak in West Africa, some nations imposed near-complete lockdowns to prevent further community contagion. The ill in those places soon became so fearful of their local hospital they did all they could to avoid any contact with it. Soon, entire hospitals had to be abandoned because they had themselves become disease transmitters.1
The COVID-19 pandemic caused profound upheaval, pain and suffering, in many ways rivaling the 1918-20 Spanish Flu H1N1 pandemic. That event infected nearly 500 million people — nearly one third of the world’s population, in four waves. Its death toll has been estimated between twenty and fifty million, ranking it among the deadliest pandemics in recorded history. The earliest cases of the 2019-2021 coronavirus pandemic were recorded in Wuhan, China, spreading to other continents with the first non-Asian outbreak occurring in Italy in early 2020. By January of 2021 100 million cases had been reported worldwide including 2.1 million deaths. In Canada alone, 747,000 cases had been reported resulting in over 19,000 deaths. The pandemic has been especially virulent in the United States, where more than 26 million cases and 500,000 deaths were reported.2 Early on, governments and medical centers, including in Israel, Italy, and New York City, sprang into rapid response mode. The Chaim Sheba Medical Center at Tel HaShomer, in the greater Tel Aviv area, quickly set up an underground 45-bed COVID-19 ICU surge hospital unit in just 72 hours in its parking garage. In Spain, two expansive halls of Barcelona’s Olímpics Vall d’Hebron municipal sports centre were repurposed into a temporary 132-bed surge hospital and the city set up two additional temporary surge hospitals in the following three weeks in repurposed arenas.3
As massive exhibition halls, sports facilities, university dormitories, retail commercial venues and even hotels were being repurposed, American examples included the Jacob Javits Convention Center in New York City, the Ernest Morial Convention Center in New Orleans, and cavernous exhibition hall spaces in Los Angeles and San Francisco. In the mad rush to rapidly respond, in any way, little time existed to ponder the matter of architecture. These enormous edifaces, combined with bare-bones provisions within, were decidedly medieval in scale and imagery. Bizarrely, Barcelona’s convention center website, Barcelona International Welcome, actually, and proudly, “marketed” its self-proclaimed social response. The Global South was similarly hit hard with virtually any available public venue taken over. In Guayaquil, Ecuador, the healthcare system completely collapsed. At the height of an outbreak there in April, 2020, bodies were crudely wrapped up in plastic and placed at curbside to await transfer to a sports stadium and then to the city morgue.4
Few saw this pandemic coming.
The public interest movement in architecture seeks to address the persistent lacuna that exists between the unmet shelter and healthcare needs of tens of millions versus what the current “system” is capable of providing. Professional architects in developed countries stand in the eye of this storm, and only when one steps away from this eye is one able to realize it is a storm of transformational import. Inadequate healthcare infrastructure, non-existent or unaffordable housing, and life-threatening ecologically degraded conditions persist. COVID-19 stirred the winds of societal unrest and misery. This public interest movement, which has been around since the 1960s, by the way, advocates for architects to not remain on the sidelines. But most architects still work mainly with and for wealthy individuals, corporations, institutions, and governments who can afford to pay professional fees and who receive, in exchange, highly tailored professional services. This modus operandi unfortunately and often tragically tends to restrict the number and types of individuals and organizations able to be served in the non-elitist public realm.
Sadly, professional architects only design about two to five percent of all buildings constructed annually in North America. This small percentage hardly supports the argument that licensed professional architects and the firms they represent do in fact attend to the public’s widespread health, safety, and welfare.5 This dilemma manifested in COVID-19. The United Nations expects the number of medically underserved worldwide to reach two billion by 2050 in a world with 9.7 billion persons.6 In tandem with this pandemic, social unrest erupted in the form of the Black Lives Matter movement, with millions losing their jobs due to economic and social displacement, potentially tumbling into housing insecurity. In this moment of such sudden (and perhaps permanent) dislocation, public interest architecture provides an alternative. One worrisome obstacle stands in the way. Sadly, there may simply be too many architects ill-trained to offer the right type of advocacy-based architectural services at the right moment.7
The coronavirus has shown that public interest, advocacy-based architecture for health is needed in partnership with the public health and medical professions. Frederick Law Olmstead was a key figure in the public health movement’s early history through his leadership of the Sanitary Commission, during the (American) Civil War (1861-1865). This organization would evolve in time into the American Red Cross. But there is recent precedent as well: in the years just prior to the coronavirus pandemic, planning, design, and public health professionals were collaborating with respect to the goal of reducing, through urban and community planning and design, the unhealthful consequences of lifestyle diseases in wealthy countries, arising from over-sedentary lifestyles. On the other end of this spectrum, joint initiatives were being directed to help mitigate severe epidemics stemming from sanitation crises in slums and shantytowns in underdeveloped nations.8 In the case of the latter it is usually the professional engineer who continues to dominate the role of main play caller, with the professional architect rarely even on the same playing field. Often, the architect is dismissed as impractical dreamer, precieved as focused on less urgent aspects of disaster mitigation such as what happened in the case of the failed efforts of the New Urbanists in the days after Hurricane Katrina in New Orleans (2005) and after Haiti’s earthquake (2010). The coronavirus pandemic provides opportunities anew to join forces with diverse client-sponsor organizations, engineers, physicians, epidemiologists, social scientists, economists, myriad specialists, and healthcare decision makers in a collective response unlike ever before.
The two aims of this review
Healthcare provider organizations, in an attempt to function as effective first responders, quickly commissioned — often, in a matter of days — an assortment of modular, prefabricated tents, containerized structures, hybrids, and myriad pop-up testing and treatment facilities in response to the accelerated spread of the coronavirus. These structures were erected adjacent to medical centers in their parking lots and in diverse site contexts. Prefabricated systems were commissioned for use as pop-up COVID-19 testing sites, laboratories, immunization units, and 24/7 ICU-surge facilities, including in the aforementioned convention centers, gymnasiums, and big box stores. A typology emerged of modular, offsite-built prefabricated COVID-19-inspired proposals and built projects; some were comissioned expressly for outdoor use, some for indoor use, and some for adaptable installation either indoors or outdoors.
Aim 1: Typological expression
To review 24 unbuilt and built projects across these four basic types:
- Redeployable walk-up/drive-up outdoor pop-up testing and/or immunization facilities, typically deployed as autonomous and self-contained (Type 1);
- Nomadic testing and immunization facilities combining a mix of vehicular with ancillary amenities such as roll-out fabric tenting (Type 2);
- Pop-up units installed in a repurposed host structure as 24/7 surge capacity ICU-based field hospitals, and quarantine housing, in a repurposed host structure (Type 3);
- Freestanding ICU-surge capacity field hospitals, and quarantine housing, installed adjacent to a medical center hospital or sited independently (Type 4).
Aim 2: Salutogenic, biophilic, and social responsibility narratives
To explore these twenty-four built and unbuilt proposals in light of the current and growing international movement to infuse healthcare architecture with salutogenic and biophilic design principles and physical amenities, including greater indoor-outdoor connectivity, a focus of healthfulness versus sickness per se, and greater personal privacy and choice. Correspondingly, a parallel aim of this review is to examine broader socio-cultural and political narratives in light of the degree to which these built and unbuilt projects express the Vitruvian precepts of architecture as entailing the provision of commodity, firmness, and delight. As such, the work of seventeen architectural firms and design collectives is reviewed, as are seven recent design studio proposals produced in the University of Toronto’s Architecture + Health graduate studio in the fall of 2020, addressing COVID-19. The pedagogical premise of the studio was that public interest architecture for medicine and public health must first begin with architectural education before it can later take root in the broader professional community.9 This design studio was taught completely online with every class meeting occurring via Zoom teleconferencing; the students were disallowed from working on campus due to provincial and City of Toronto COVID-19 restrictions. Under the direction of this author, student projects are reviewed below. Restated, this built and unbuilt work is reviewed through the lens of its typological, salutogenic and biophilic narratives, and for its advocacy of socially responsible public interest architecture.
Type 1: Pop-up COVID-19 testing and immunization units
Eight Type 1, Type 2 and Type 3 unbuilt and built proposals are reviewed below, followed by three Type 3 University of Toronto Architecture + Health graduate studio proposals:
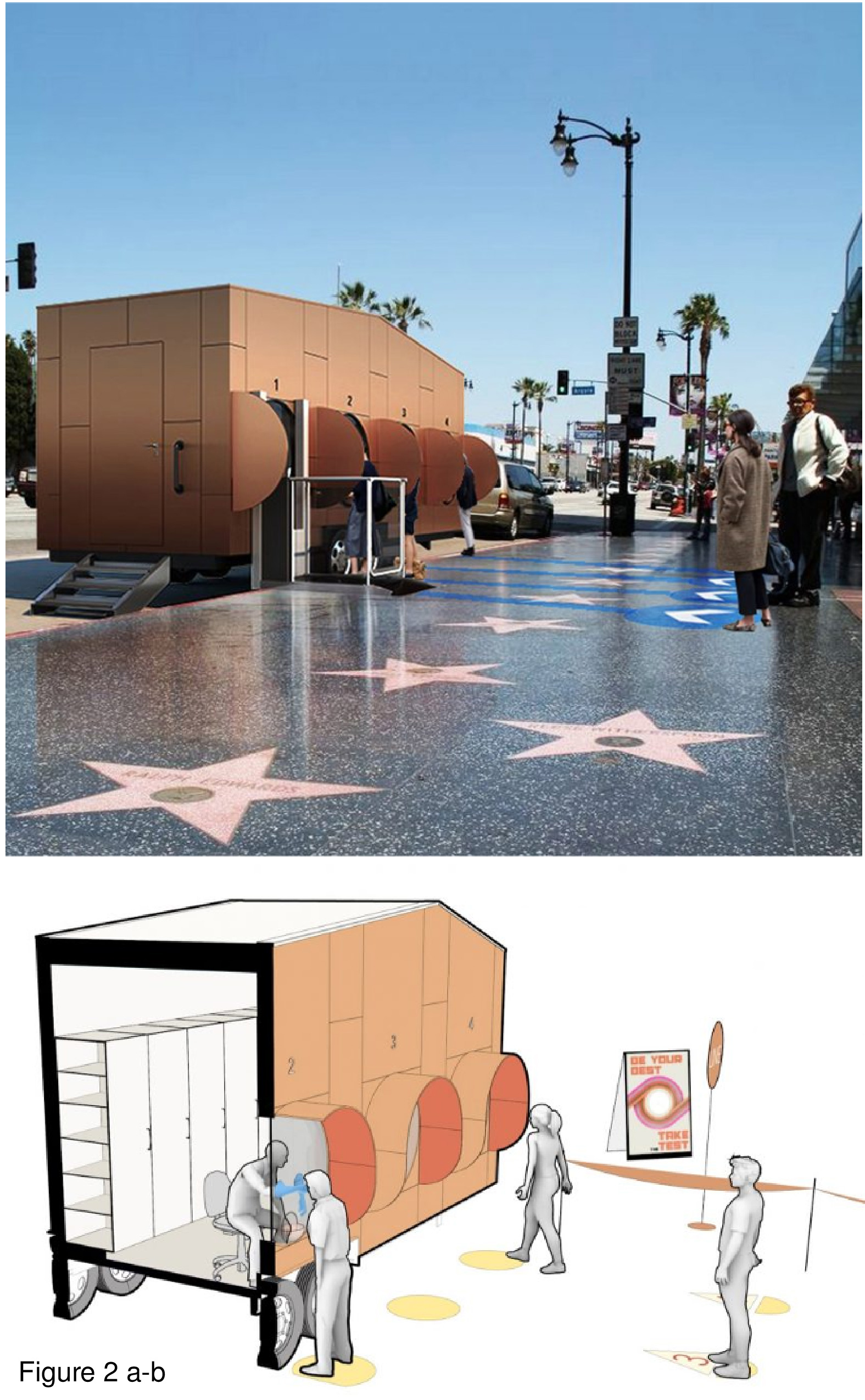
Covid-19 Mobile Unit
Firm: M-RAD, Santa Monica, CA USA
Images: Courtesy M-RAD.
This modular unit is essentially a trailer that is pulled by another vehicle. It is fabricated in lightweight steel and depicted here in a salmon hue with the option to imprint patterns and textures on the outer panels. It features three testing stations, each with a window with circular pass-through portal. An outward-projecting panel affords a modicum of privacy and serves as infection control device. The unit is staffed by three nurses. A portable lift allows for an individual in a wheelchair to be elevated to standing height in order to administer a COVID-19 nasal swab test (CNST). This prototype is not equipped for immunizations on-board the unit. The unit is shown deployed throughout Los Angeles, including in well-known settings such as on the Santa Monica Pier, along Beverly Hills’ Rodeo Drive, and on the sidewalk of Hollywood Walk of Fame. At night, the installation is dependent on external (streetlamp) illumination. It is almost as if one were walking up to casually order a hot dog, fries, and Coke at the famous Tail O’ the Pup hot dog stand, an iconic commercial vernacular fixture in Los Angeles since the 1930s.10 (Figure 1 and Figure 2a-b.)
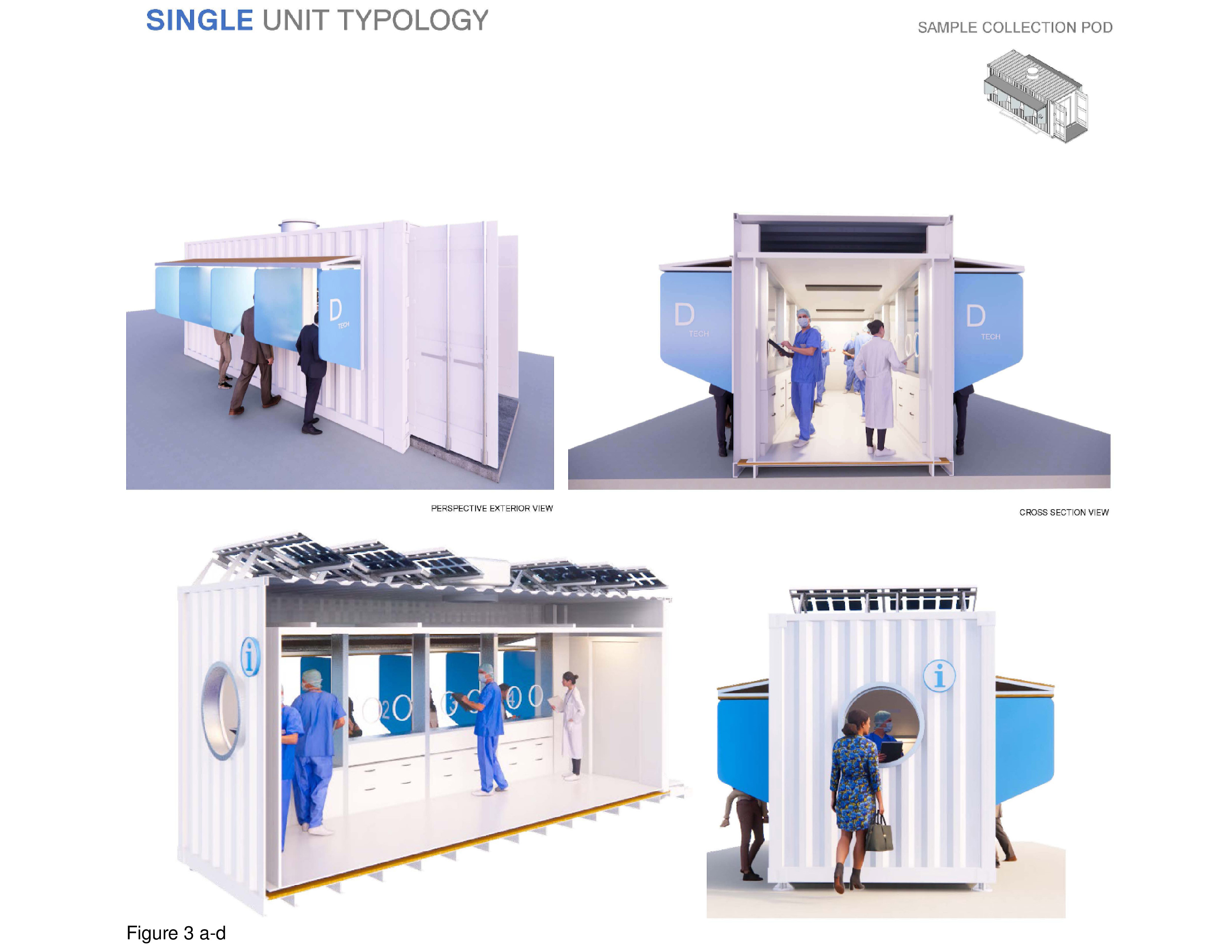
Prefab Covid-19 Test Center
Firm: Grimshaw Architects w/SG Block and Osang Healthcare, USA
Images: Courtesy Grimshaw Architects
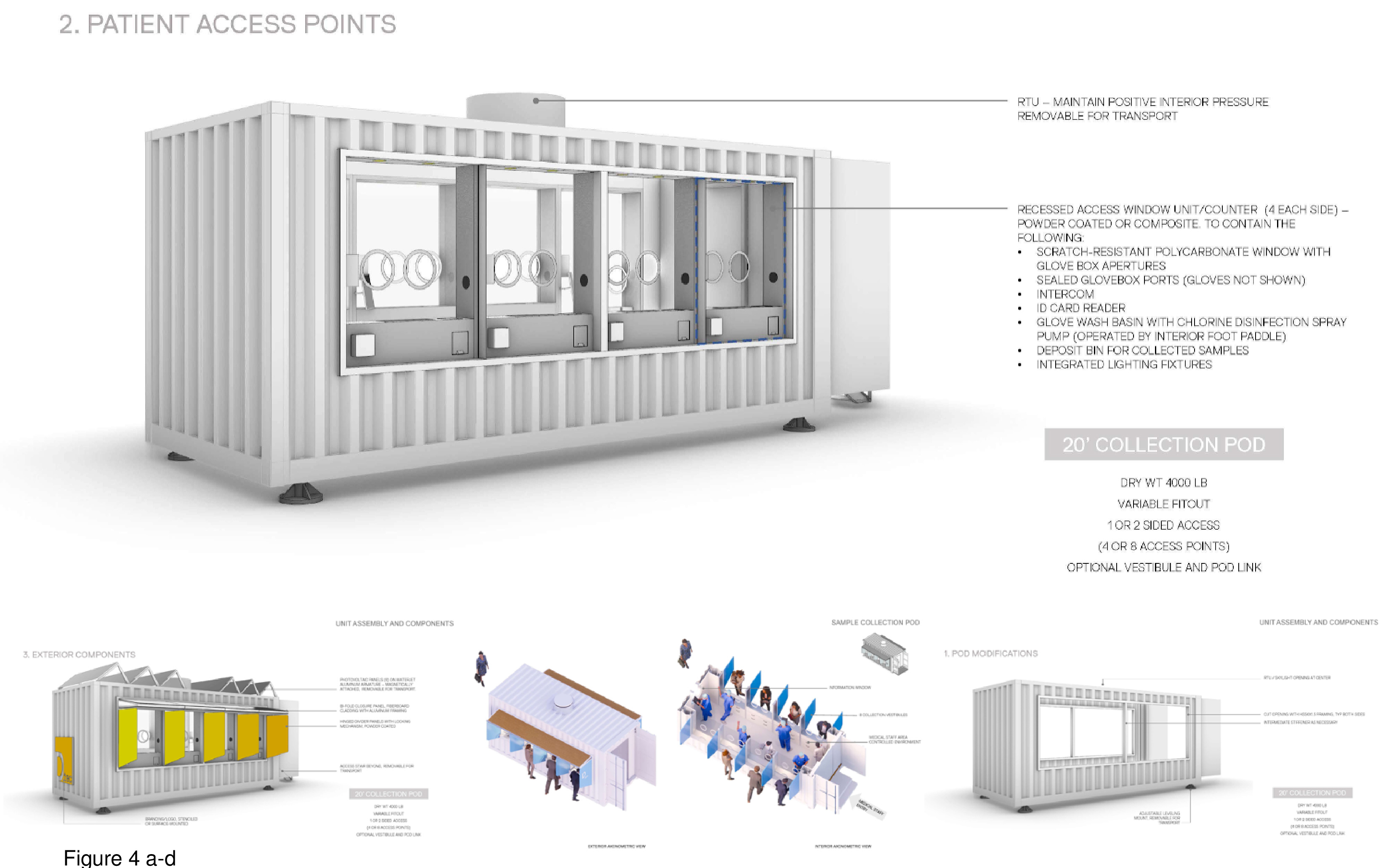
This 20-foot custom-built intermodal shipping container features a bank of solar panels on the roof; the panels are installed on-site. It features eight walk-up testing stations, A/B/C/D, four on each side of the container unit. A window with circular opening is provided for administering the CNST. The testing stations are partially shielded from one another by means of projecting panels. The overall white colour of the container unit contrasts its colour-accented banding. Additional panels can be installed as a roof-sunscreen. One end of the unit has a sign-in/point of contact window, with a staff entrance provided on the opposite end. The staff housed inside would appear to be rather cramped, with little space for medical equipment, including personal protective equipment (PPE), administrative workspace/desks, or storage of patient specimens. A roof vent ensures the unit’s continuous negative air pressurization. The unit sits slightly off the ground plane.11 The unit shown here does not appear equipped to provide immunizations inside the container. (Figure 3a-d and Figure 4a-d.)
Citizen Care Pod, Canada
Firms: WZMH Architects, PCL Construction, Insight Enterprises and Microsoft, with Parkin Architects, Toronto
Photos/Images: Courtesy WZMH Architects and PCL Construction.
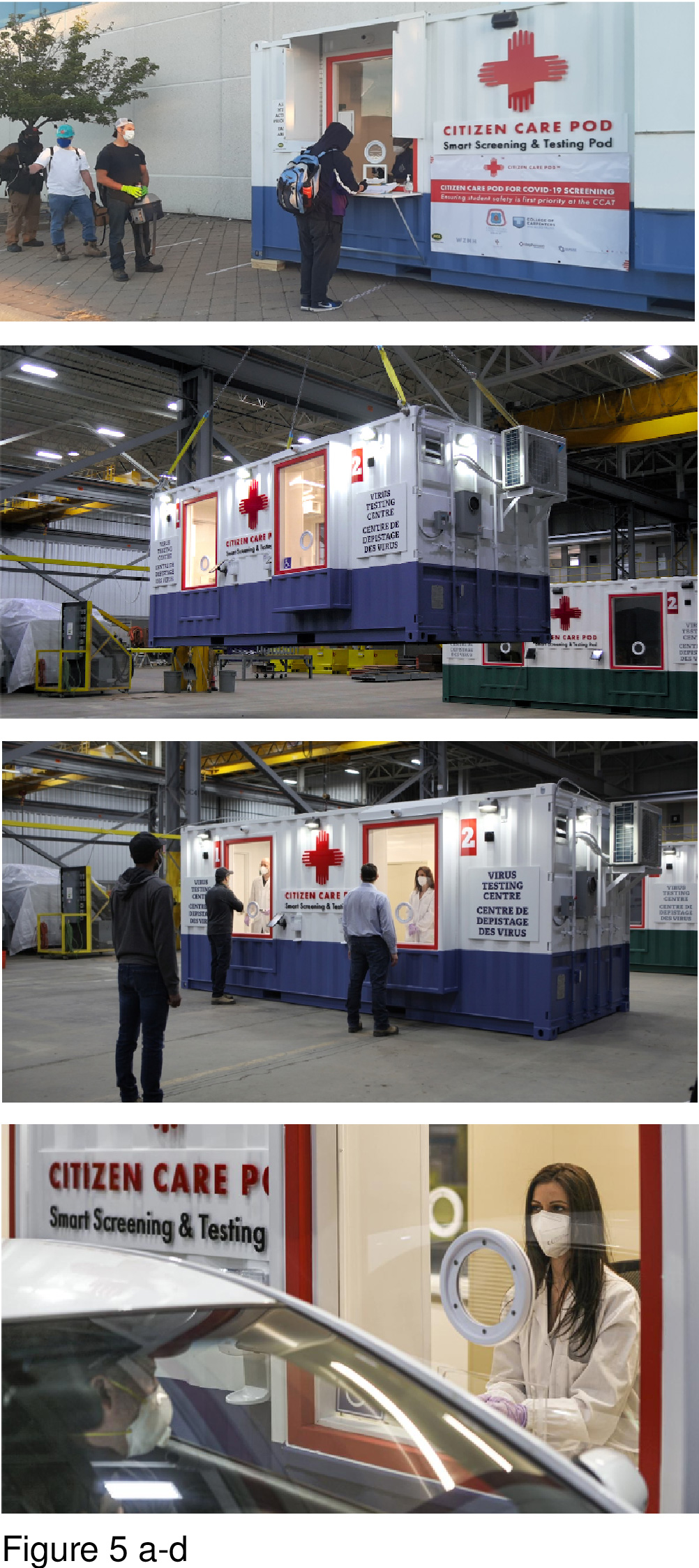
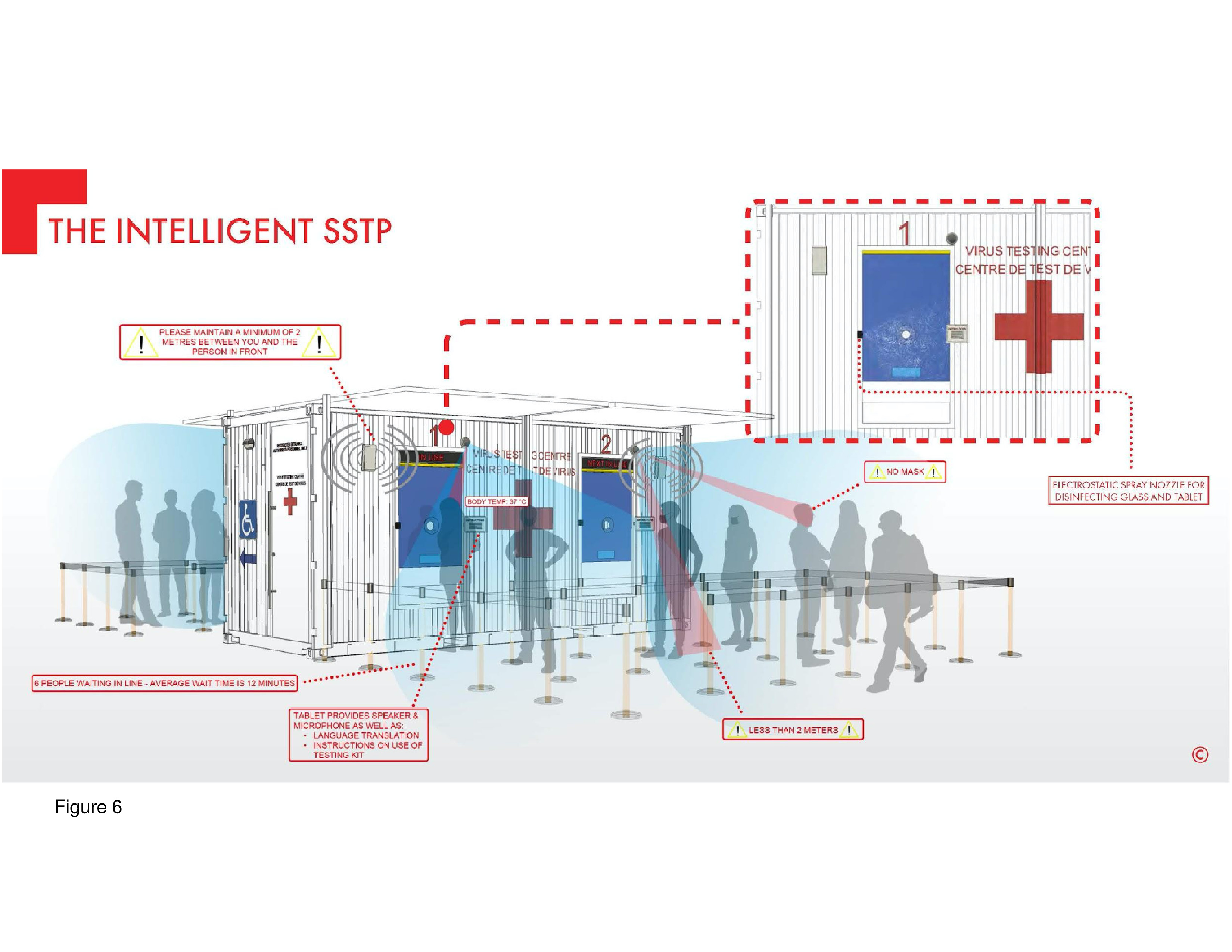
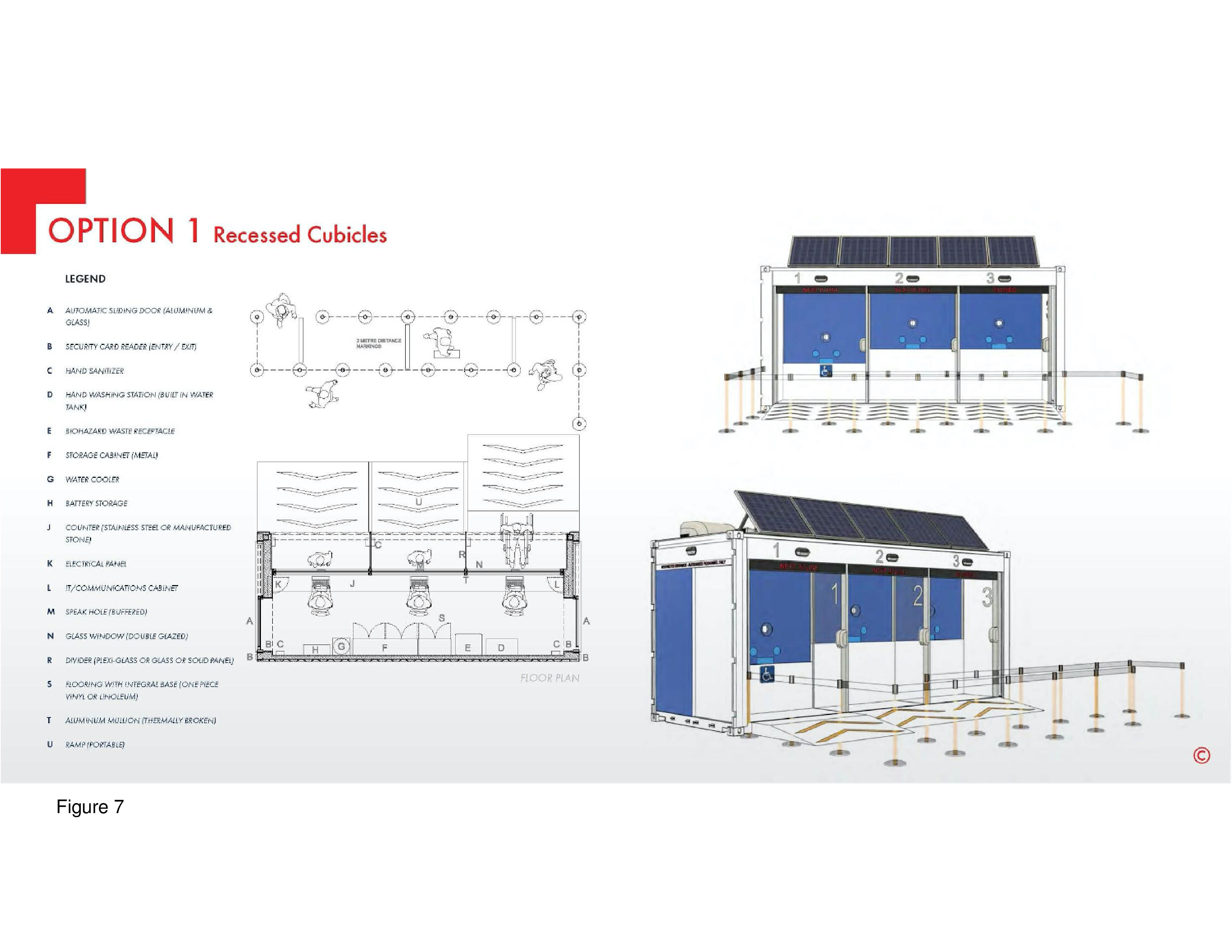
This built prototype is based on the standard modular intermodal shipping container. The white and blue exterior provides backdrop to the international Red Cross logo, readily visible. It is adaptable to various site contexts and functional needs, is reconfigurable, and can be quickly installed. Testing stations are separated by a projecting, diagonal steel panel with the number of the testing station provided . Negative air pressurization is maintained by means of an external clip-on HVAC unit. Six design options are shown on the firm’s website: With and without roof solar panels; with “outboard” walk-up testing stations; with an inset outer wall panel presumably to protect patients from the elements; with a drive-up window for testing; another with a pass-through portal for CNST; as a single-occupancy “phone booth” where the patient stands outside; and as a double or triple-length hybrid installation for testing, immunizations, with an on-board laboratory. The Citizen Care Pod is highly adaptable.12 An additional option shown on the firm’s website is an elevated step-up unit, such as the installation at Vancouver’s airport, in British Columbia. (Figure 5a-d, Figure 6 and Figure 7.)
Type 2: COVID-19 vehicular nomad units
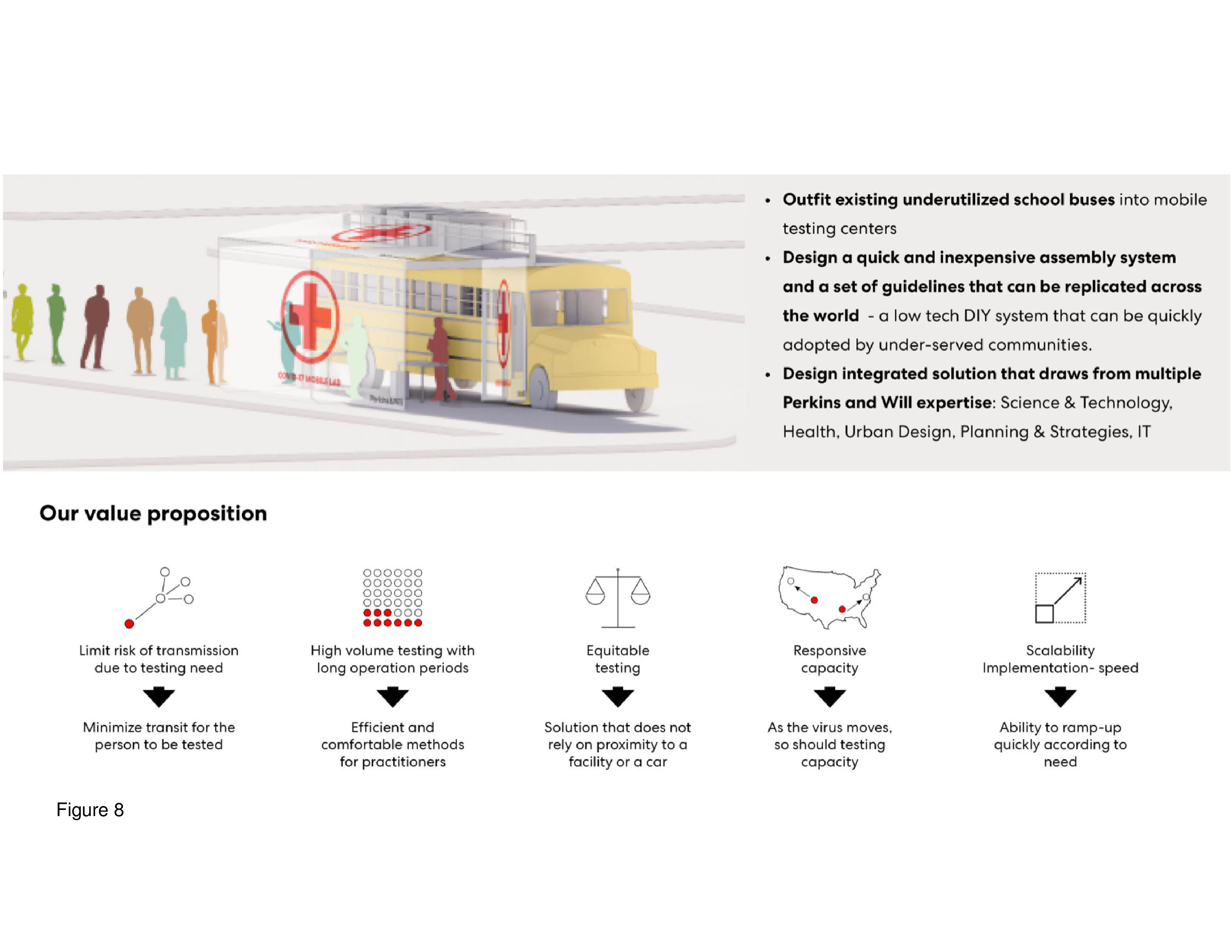
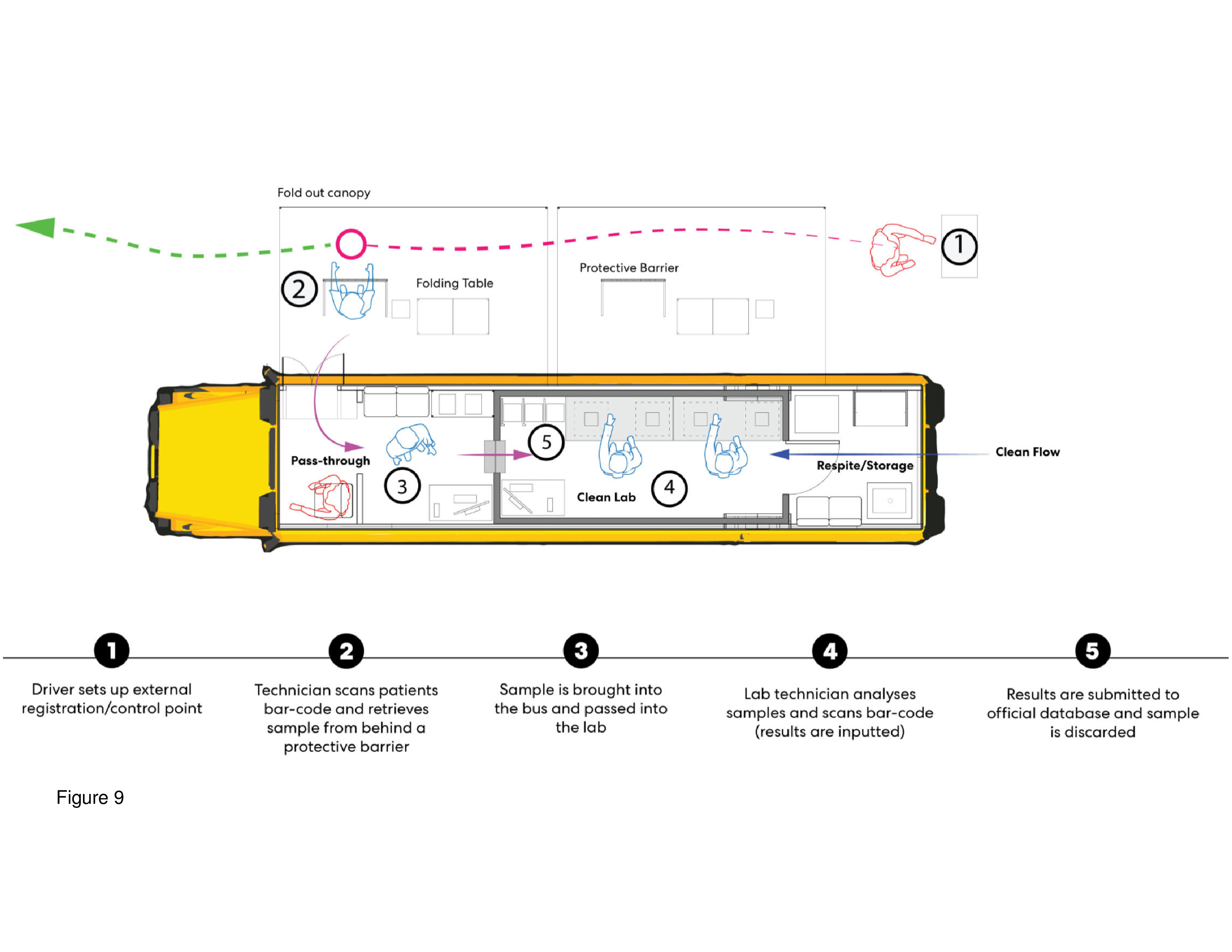
Mobile Testing Center
Firm: Perkins and Will/Schmidt Hammer Lassen/ARUP Group, USA
Images: Courtesy Perkins and Will.
Here, a conventional school bus is converted into a rolling COVID-19 testing and immunization unit. This relatively inexpensive concept calls for the repurposing of a fleet of conventional school buses and then sending them out to schools and other locations in the hinterland. This bus-cum-clinic can be quickly deployed to medically underserved communities, and this is perhaps its main advantage as well as the fact it is self-powered. A fleet of repurposed buses is expandable by simply adding more units. The driver doubles as the point of contact, and a technician scans patients’ barcode data and then administers the CNST through a plastic protective membrane barrier/window. The extracted specimen can be processed in the on-board lab with the result quickly recorded via barcode technology into a central database. The interior of the bus is subdivided into three compartments: administration/registration/testing, laboratory, and staff work/PPE storage zone. Outside, a pull-out canvas tent protects patients from the elements, with tables and chairs provided beneath. This outdoor “room” functions as both waiting and testing/immunization staging area.13 (Figure 8 and Figure 9.)
Type 3: COVID-19 Pop-ups in repurposed host structures
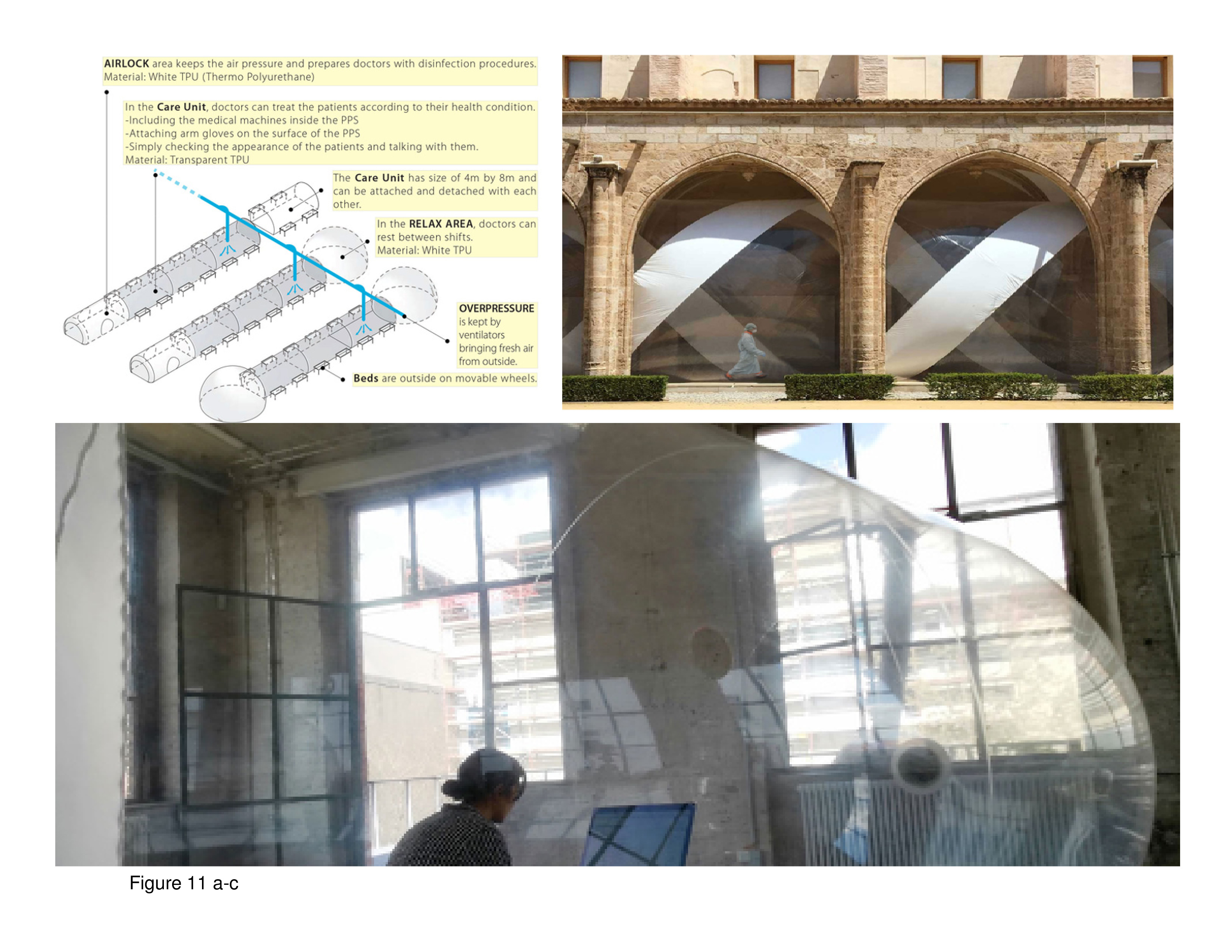
PPS (Personal Protective Space) for Caregivers
Firm: plastique fantastique Art Group, Berlin, Germany
Photos/Images: Courtesy plastique fantastique.
This proposal reprises the bold, visionary proposals put forth by E. Todd Wheeler at Perkins+Will in the 1960s — intersected with the utopian/dystopian proposals put forth by Archigram, from this same period. Archigram was an iconoclastic, London-based art-architectural firm. Other so-called utopian proposals from the same period included pneumatic transport tubes, with one memorable unrealized proposal standing out: the patient spends her/his entire hospital stay inside the same clear-Plexiglas capsule, equipped with lift-hatch access panel. This capsule module was to be transported by means of an extensive ceiling-mounted rail network from diagnostic and treatment station to station. The aim was to render the traditional patient room completely obsolete in the International Style high-tech machine megahospital. These clear plastic capsule shells were shaped like a dosage capsule.14 In the case of the PPS for Caregivers, by contrast, a soft plastic pneumatic bubble is occupied by staff personnel with a small opening provided in the bubble for administration of CNSTs. The patient sits on a chair outside the clear plastic bubble. On the firm’s website multiple bubble-tubes are shown installed in repurposed host buildings. The installation shown here is in an open loft in a repurposed museum. Pnumatic tubes are inflated by continuous negative air pressurization and more tubes can be added, creating linear wings connected by a support spine-tube. Curiously, patient beds are shown outside the bubble-tube. What of patient privacy, confidentiality, and most importantly, infection control?15 (Figure 10 and Figure 11a-c.)
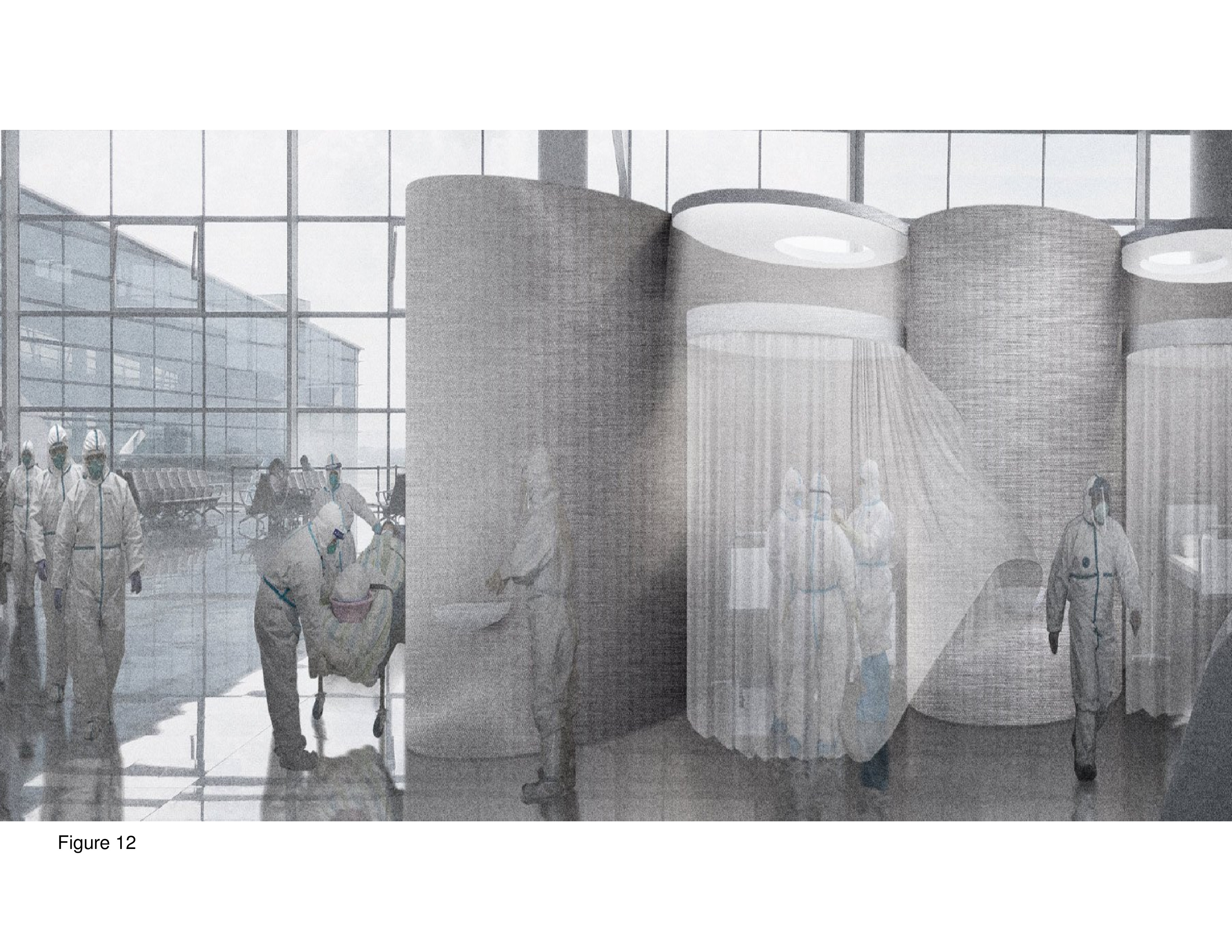
COVID-19 Superhospital
Firm: Opposite Office, Munich, Germany
Images: Courtesy Opposite Office
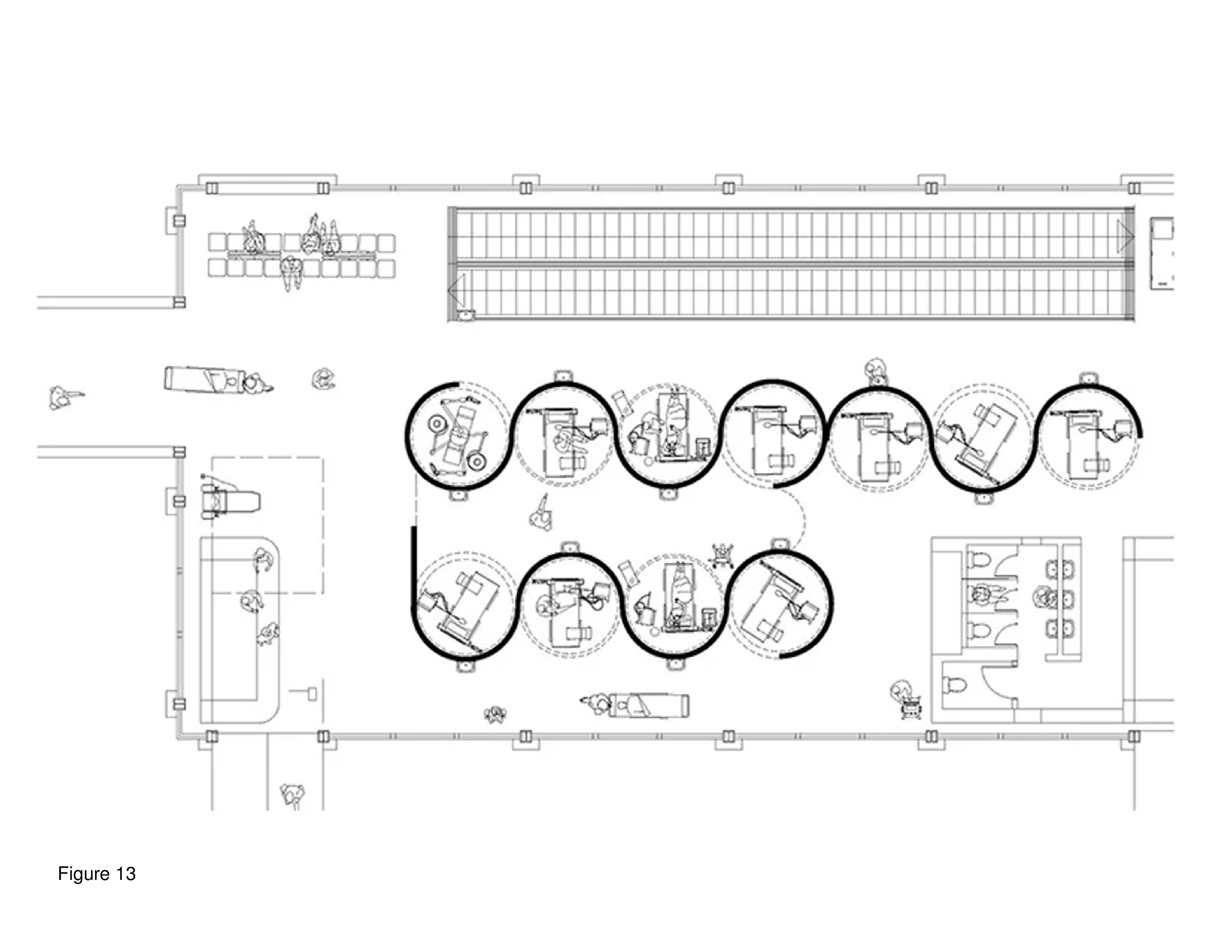
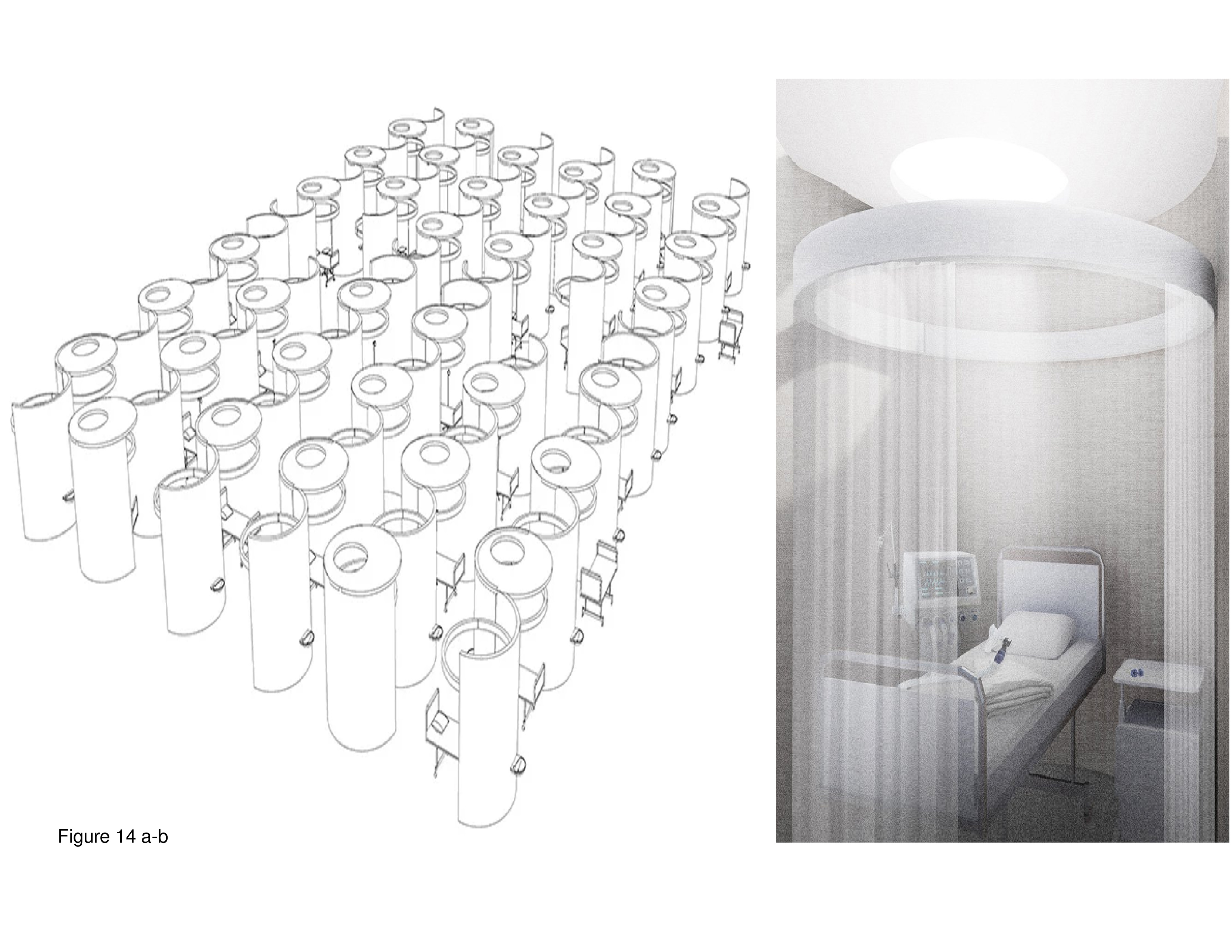
This prototype is shown installed in the problem-plagued Brandenburg International Airport that recently opened in Berlin. This pop-up is installed in a terminal close in proximity to where travellers board and deplane. With international air travel so drastically curtailed, many airports installed onsite testing units to control community contagion and for the distribution of PPE. This proposal, stark in imagery, consists of dozens of close-packed semicircular modules with each module fabricated of Plexiglas. Semicircular patient modules are equipped with white fabric pull curtains. The walls of the modules repetitively interweave in an interlocking pattern. Patient room and diagnosis and treatment modules are decentralized, in plan. The existing HVAC, electrical, plumbing systems and restrooms in the airport terminal are, presumably, repurposed in support of the COVID-19 Superhospital. The installation is a honeycombed network and the vast height of the terminal’s roof above allows for the modules’ relatively high ceilings. Question: Is the somewhat dark, neo-Gothic imagery of this pop-up indicative of what a hospital room in heaven might look like?16 (Figure 12, Figure 13 and Figure 14a-b.)
CAMP-15, Kulturpark, Turkey
Firm: !NFEKT, Ankara, Turkey
This pop-up is shown installed in repurposed host structures, for the administration of CNSTs and to accommodate patient overnight observation. This prefab modular system is depicted in a grid configuration inside a large industrial warehouse. Dozens of modules are arranged repetitively in long rows yielding double loaded circulation paths, and the roof of the host’s ceiling is visible from within the modules. Staff workspaces are interspersed between the patient rooms, observation areas, and assessment spaces. Some are directly visible by passersby in the adjacent corridor. One distinguishing feature of this system is its siting within a central-city district near a major medical center.17 (Images not shown.)
COVID-19 Testing Center and Laboratory, Shijiazhuang, China

Photo: Courtesy of Yang Shiyao/Xinhua and the Associated Press
In January of 2021 more than twenty-two million people were ordered to remain in their homes in three cities in China — double the number of citizens the central government ordered locked down the January before in Wuhan. Wuhan was where the coronavirus was first reported in China in late 2019. When this second lockdown was ordererd in Shijiazhuang the local public health authorities mandated the collection of more than ten million CNSTs over the next three days, totaling nearly one per resident. Test specimens were immediately sent to this and other pop-up labs quickly installed inside repurposed host structures.18 As shown, ten barrel-vaulted, pneumatically-supported units are configured in five rows. Each module is structurally autonomous, with its own HVAC system to ensure negative air pressurization. A sign-in window is staffed to receive test samples. This vinyl-sheathed system is manufactured for indoor as well as outdoor installations. (Figure 15.)
University of Toronto Architecture + Health Graduate Design Studio
Project 1: COVID-19 pop-up units in repurposed host structures
In the fall of 2020, the Architecture + Health studio produced proposals for a prefab pop-up testing and immunization unit for installation in repurposed host structures in the Greater Toronto Area (GTA). Hosts ranged from temporarily shuttered gyms in community recreational centres, retail commercial structures, churches, a terminal at Pearson International Airport, a YMCA, and an art museum. The brief called for a lift-pack system, with an arrival, registration, and waiting area, five CNST rooms, five rooms for immunizations, workspace for staff personnel, service entrance, and plug-in power generation for negative air pressurization. This lift-pack system must be able to be transited via truck. IT, HVAC, electrical, and plumbing systems run beneath a raised platform with ramp and stair access. The modules feature lighting units suspended from an open grid, which also facilitates air flow. Internal circulation isolates non-symptomatic from symptomatic individuals. Parking is provided on site as is space for individuals to queue outdoors weather permitting. Wherever HVAC, plumbing, and electrical system requirements cannot be provided by the host, support infrastructure is brought onsite. In healthcare facilities, behaviours and situations that are mentally fatiguing, requiring prolonged, intense concentration with few breaks, can be highly stressful. Windowless conditions are but one example of how sensory deprivation can have a deleterious effect on health status. The brief therefore called for incorporating salutogenic and biophilic design principles and concepts. Specifically, this included a theoretical premise put forth by the late environmental psychologist, Stephen Kaplan, Attention Restoration Theory (ART). This theory posits that humans need positive distractions from stressful circumstances and that psychologically meaningful engagement with nature is one way this can be achieved. 19 This studio project was six weeks in duration and students worked in four teams of two students. A dozen leading healthcare design professionals in Canada and the United States participated in design reviews during the project via zoom teleconferencing. This external reviewer format continued throughout the second project of the fall 2020 term (discussed below). Three testing/immunization pop-up proposals are presented here:
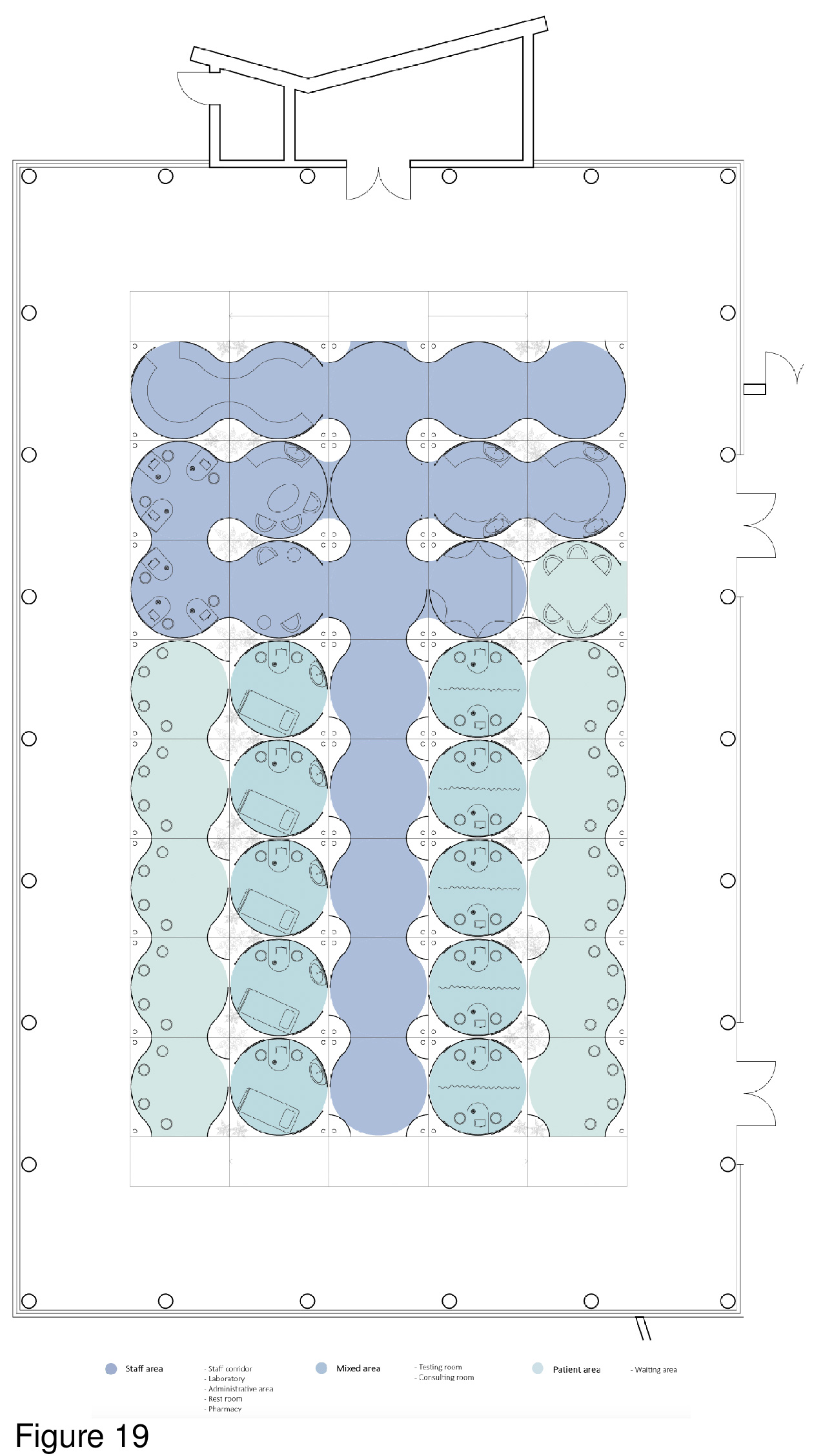
Transparency and Health
Zohar Nekouian Fathi and Yijie Dai
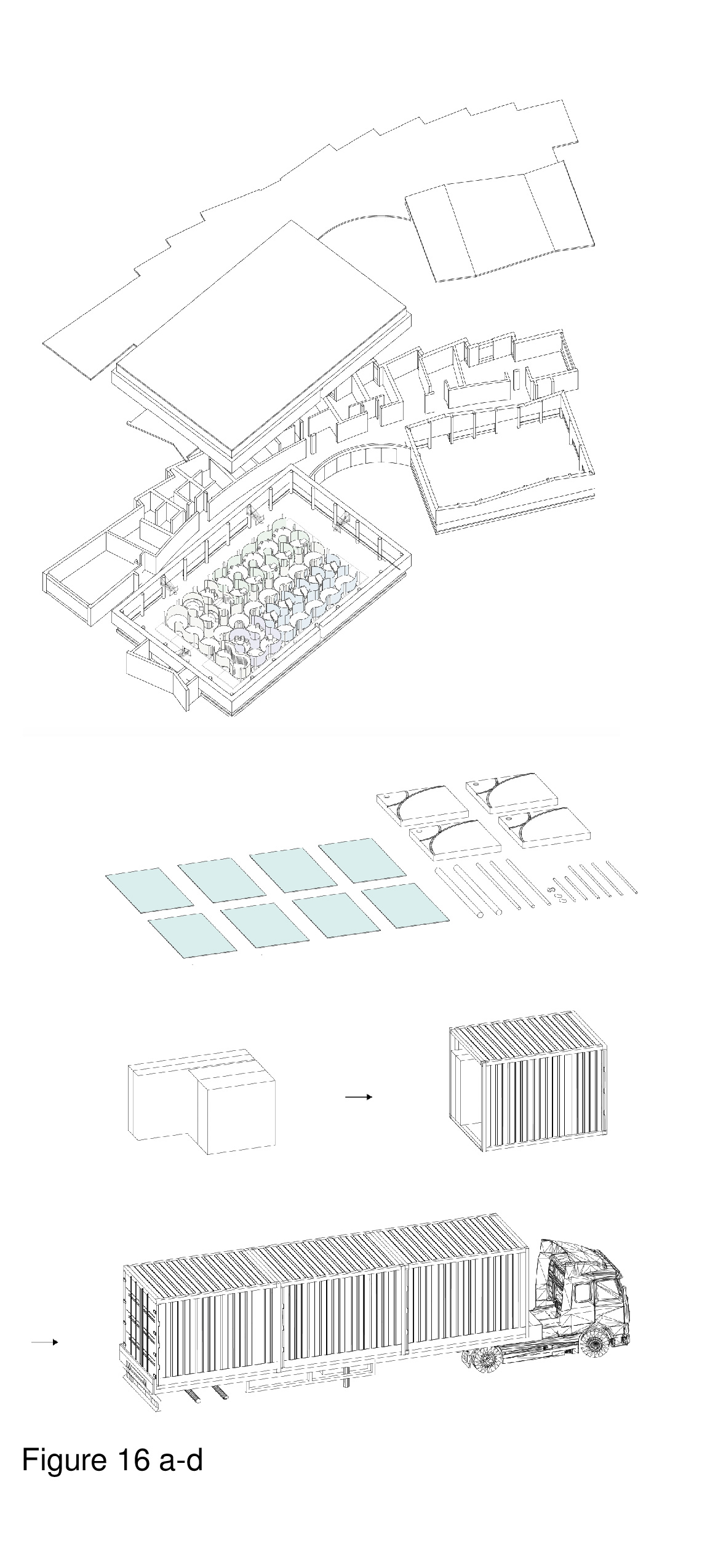
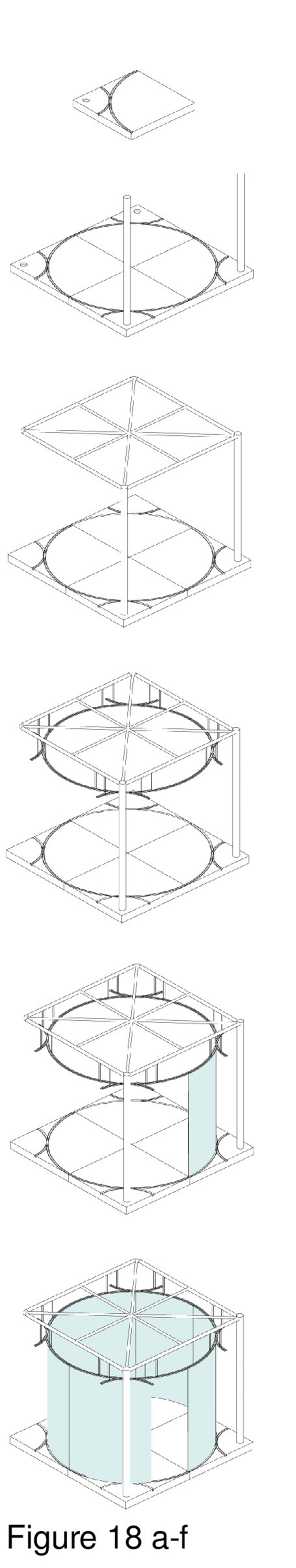
Many outpatient health clinics are needlessly institutional, with windowless waiting areas, examination rooms, treatment rooms, open-plan staff cubicles, and dreary corridors. Visual interconnectivity between a clinic’s constituent rooms and zones is minimal at best. This pop-up installation rejects drab institutionalism in favour of colour, transparency, and non-orthogonality. System componentry is transited to the host in standard shipping containers, is brought indoors and erected. The host shown here is a pneumatically-supported recreational sports facility built in 2012 in a suburb of Toronto. Modules are circular with interlocking curvilinear walls, fabricated in a mix of full-height translucent and opaque polycarbonate panels. The various types of panels provide differing degrees of transparency, affording privacy as required, while allowing light to penetrate the interior. The system is comprised of close-packed modules identical in plan configuration, with colour-coded zones. (Figure 16a-d, Figure 17a-f, Figure 18a-f, Figure 19 and Figure 20.)
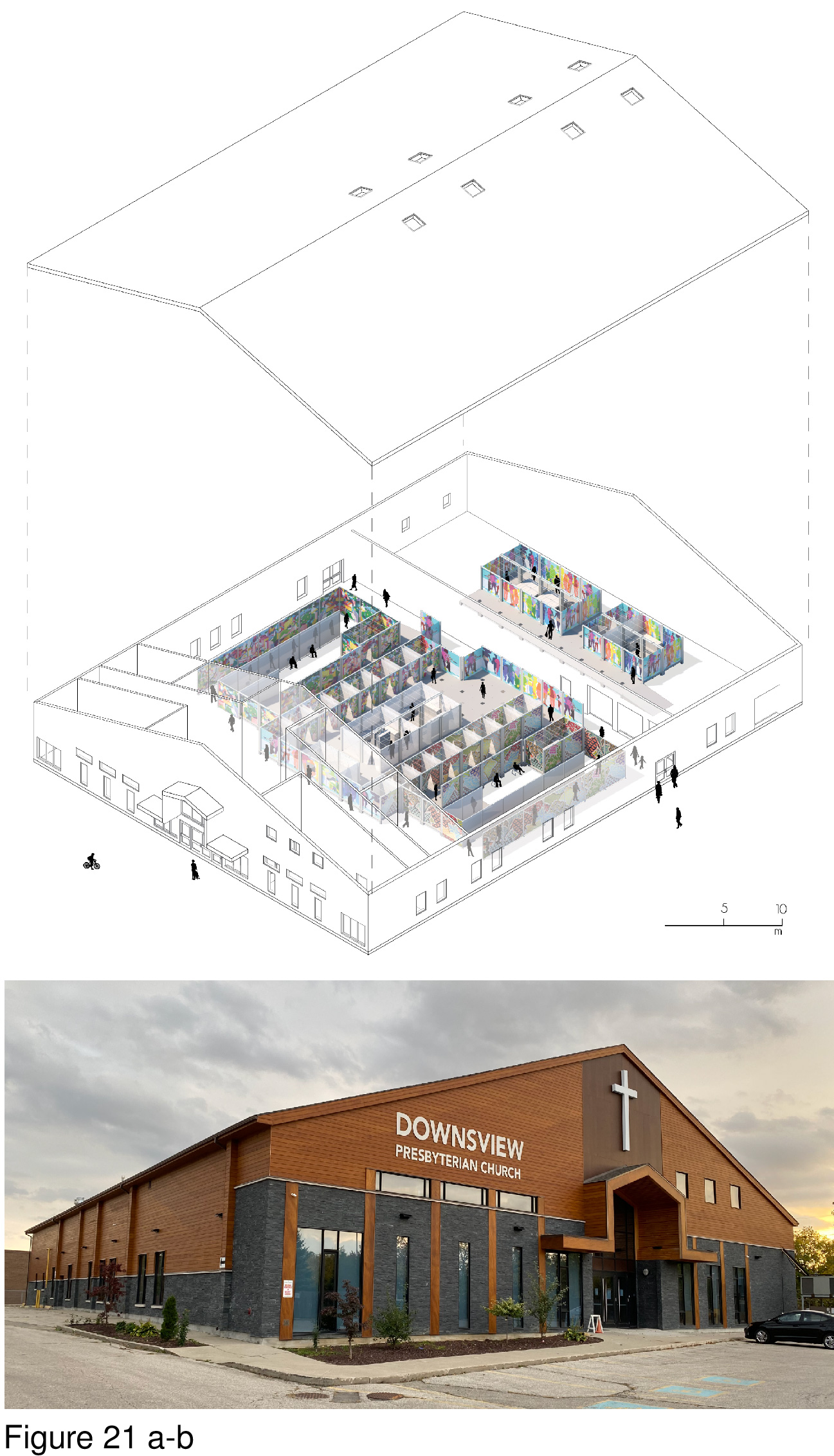
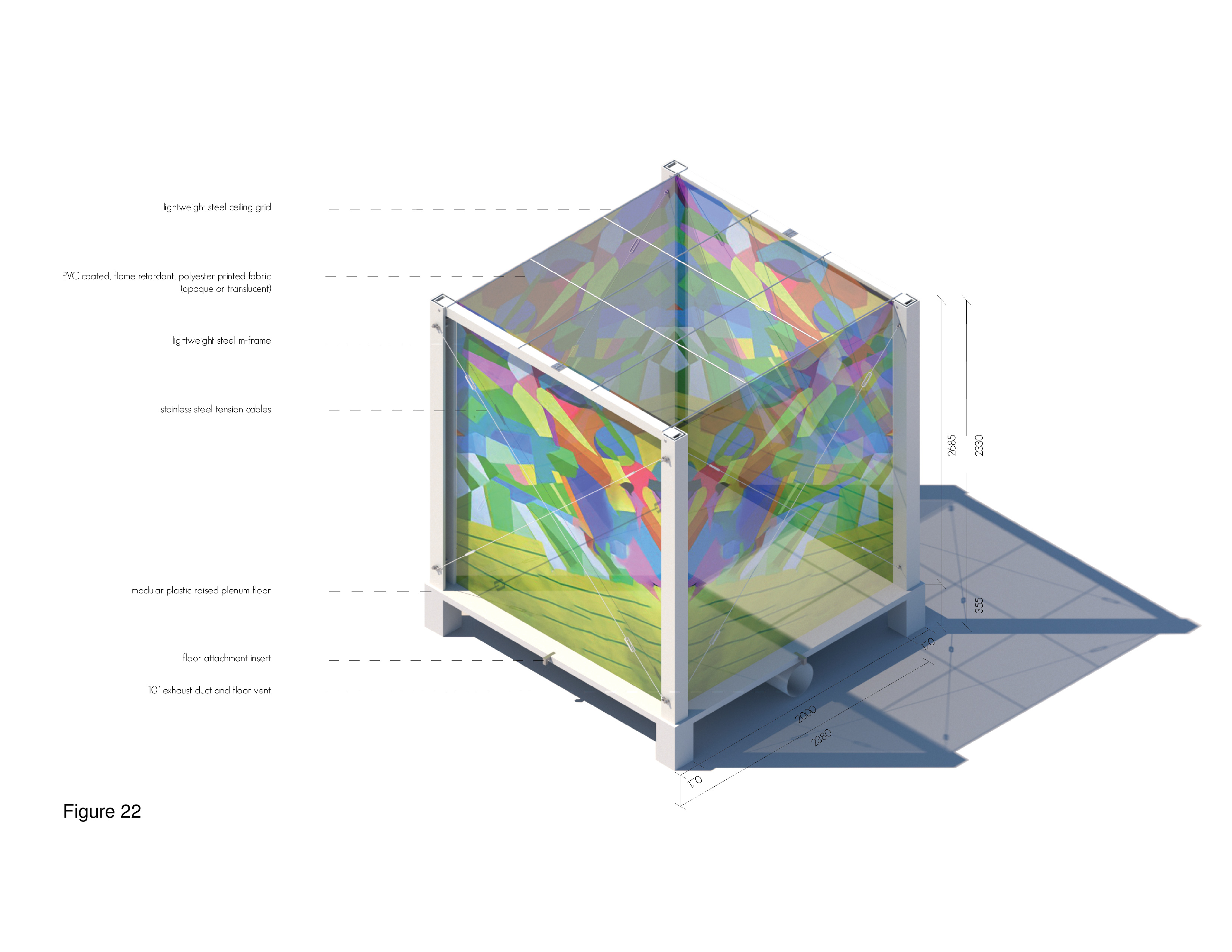
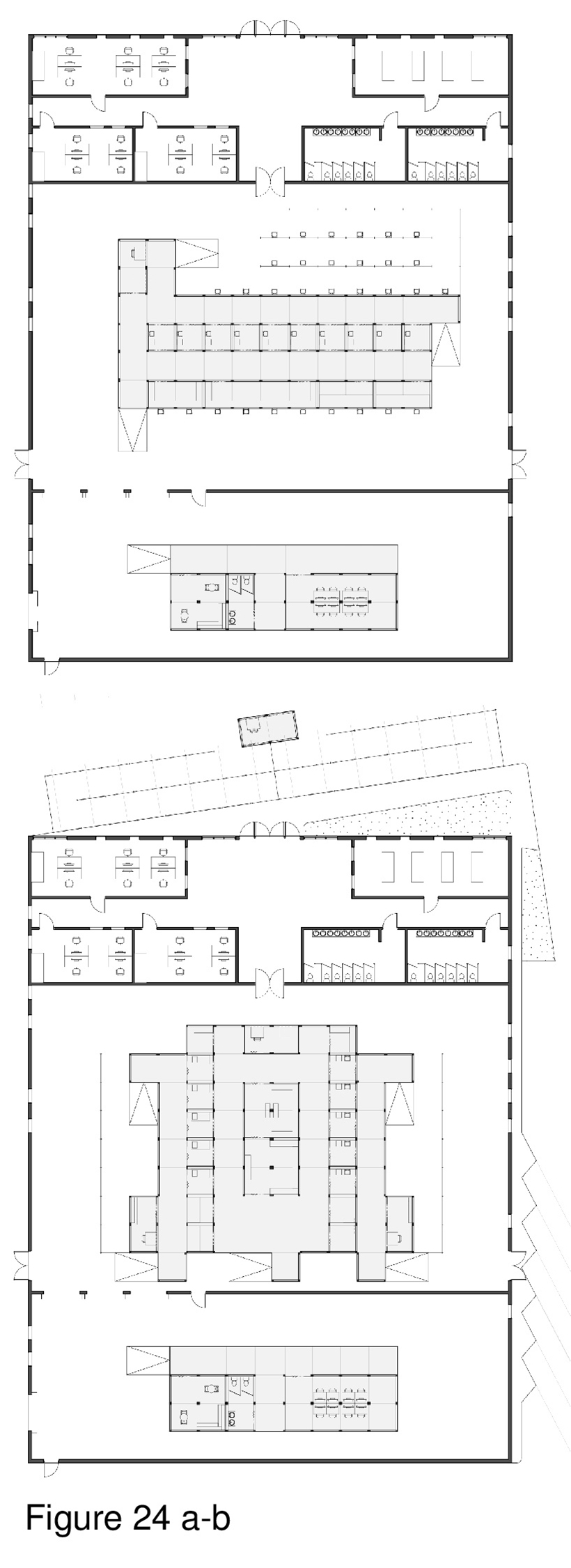
Art Therapy and Health
Bronte Morris-Poolman and Damian Kercz
Governments and healthcare organizations were in crisis mode to respond rapidly and art per se was not top of mind. That said, humans derive therapeutic benefit from attentional diversity and the ability to transition when necessary from voluntary cognitive behaviours (taxing, requiring concentration) to involuntary (liberating, enjoyable) cognitive behaviours and activities — healthcare built environments notwithstanding.19 Recent evidence-based research has found art to be a source of therapeutic affordances to patients, caregivers, and patients’ families. This type of positive stimulation has been empirically linked with a reduction in stress. Accordingly, Attention Restoration Theory (ART) inspired the design of this lift-pack system featuring the work of established and rising Toronto artists. Artworks are presented on translucent polycarbonate panels facing circulation paths and in public zones. Here, a church is shown repurposed as a grid in plan. Judicious placement of art panels throughout the installation creates a series of unexpected, positive distraction events. This is underscored by footlights installed in the floor panel, and by downlighting installed on the ceiling of the host structure. The intent is to help alleviate some of the sheer mental fatigue and stress associated with COVID-19. (Figure 21a-b, Figure 22, Figure 23a-b and Figure 24a-b.)20
Biophilia and Health
Emily Moore and Jiawen Lin
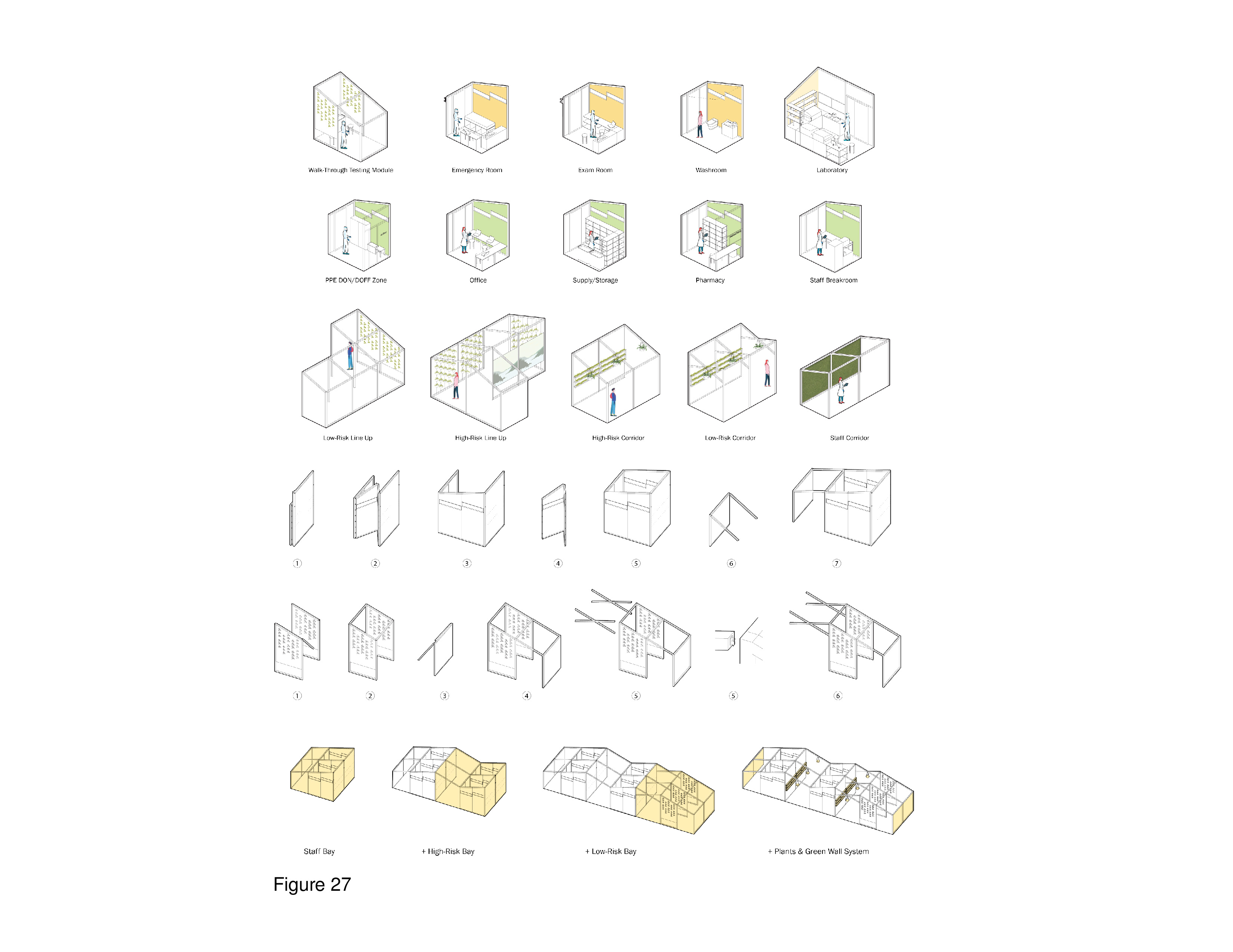
The Biophilia Hypothesis, first postulated by Edward O. Wilson (discussed below), has garnered much attention of late. This theory assumes that humans, as a species, possess a strong evolutionary predilection for meaningful transactions with nature and landscape.21 Biophilia theory has been elaborated upon by Stephen Kellert and others more recently.22 Its application in the built healthcare environment has been researched in the past decade.23 Recent evidence-based research on biophilia centers on the positive psychological benefits of nature and landscape on human well-being and health outcomes,24 has resulted in design recommendations,25 and even includes a call for its inclusion as a baseline metric in architectural design excellence award and certification programs, including LEED.26 In accord with attention restoration theory, this pop-up incorporates nature imagery on polycarbonate wall panels attached to a cube-frame. This frame is reconfigurable based on changing functional requirements. The host shown is a vacant liquor store in Toronto’s urban core, near a major intersection, with onsite parking and near public transit. The installation is a grid, in plan, with modules supplied by HVAC, plumbing and electrical support from below a platform floor. Patients encounter representational nature content upon first arrival and throughout, including in examination and immunization modules. The polycarbonate panels depict abstracted fauna and outdoor scenes, at times supplemented by real plants. (Figure 25a-f, Figure 26a-b and Figure 27.)
Type 4: COVID-19 Lift-pack and containerized surge field hospitals and quarantine units
Nine unbuilt and built Type 4 projects are reviewed below, followed by four University of Toronto Architecture + Health graduate studio proposals:
QurE
Firm: NCKU and Bio-architecture Formosana (BAF), Taipei, Taiwan
Photos/Images: Courtesy BAF
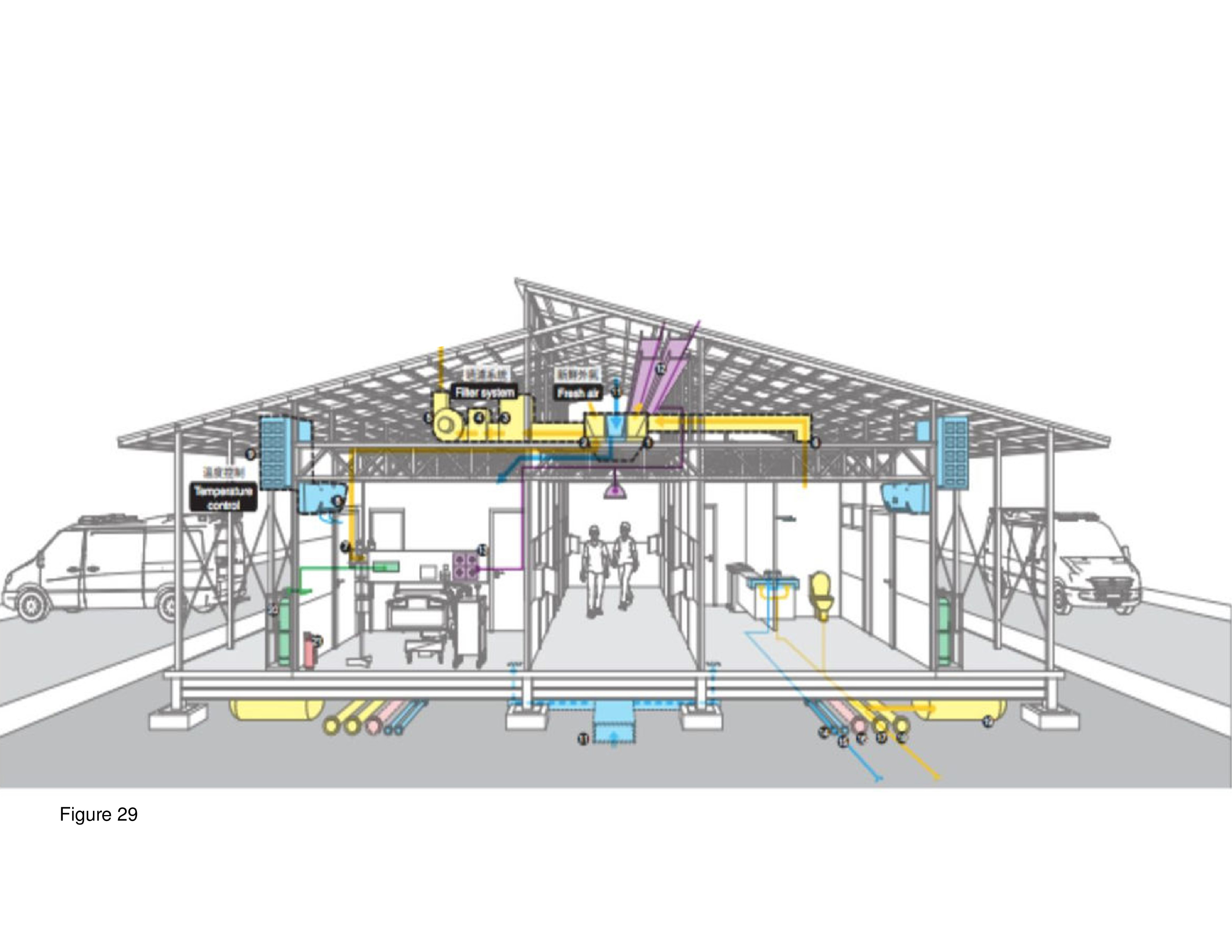
The QurE (Quarantine Unit for Recovery, Emergency and Ecology) prototype is a prefab emergency quarantine and medical treatment shelter for COVID-19. It was unveiled April of 2020 at the National Cheng Kung University in Tainan City, Taiwan. QueE was jointly developed by NCKU and Taipei-city based BAF. Construction documents and specifications are available through online open access. It was a joint venture between academia and private industry, is constructible in three days, and adaptable to irregular terrain. Airtight floor and wall panels, metal alloys, and thermal insulation ensure continuous negative air pressurization. The goal of the system is to isolate the infected patient in an intensive medical care setting. Natural daylight is transmitted to the interior, with perimeter and double loaded circulation provided. Patient isolation rooms are across from the toilet/shower unit. This system is expandable as needs dictate. This prototype was on public display on NCKU’s campus in the Spring of 2020.27 (Figure 28 and Figure 29.)
Modular Mobile Hospital
Firm: VHL Architecture, Da Nang, Vietnam
Images: Courtesy VHL Architecture.
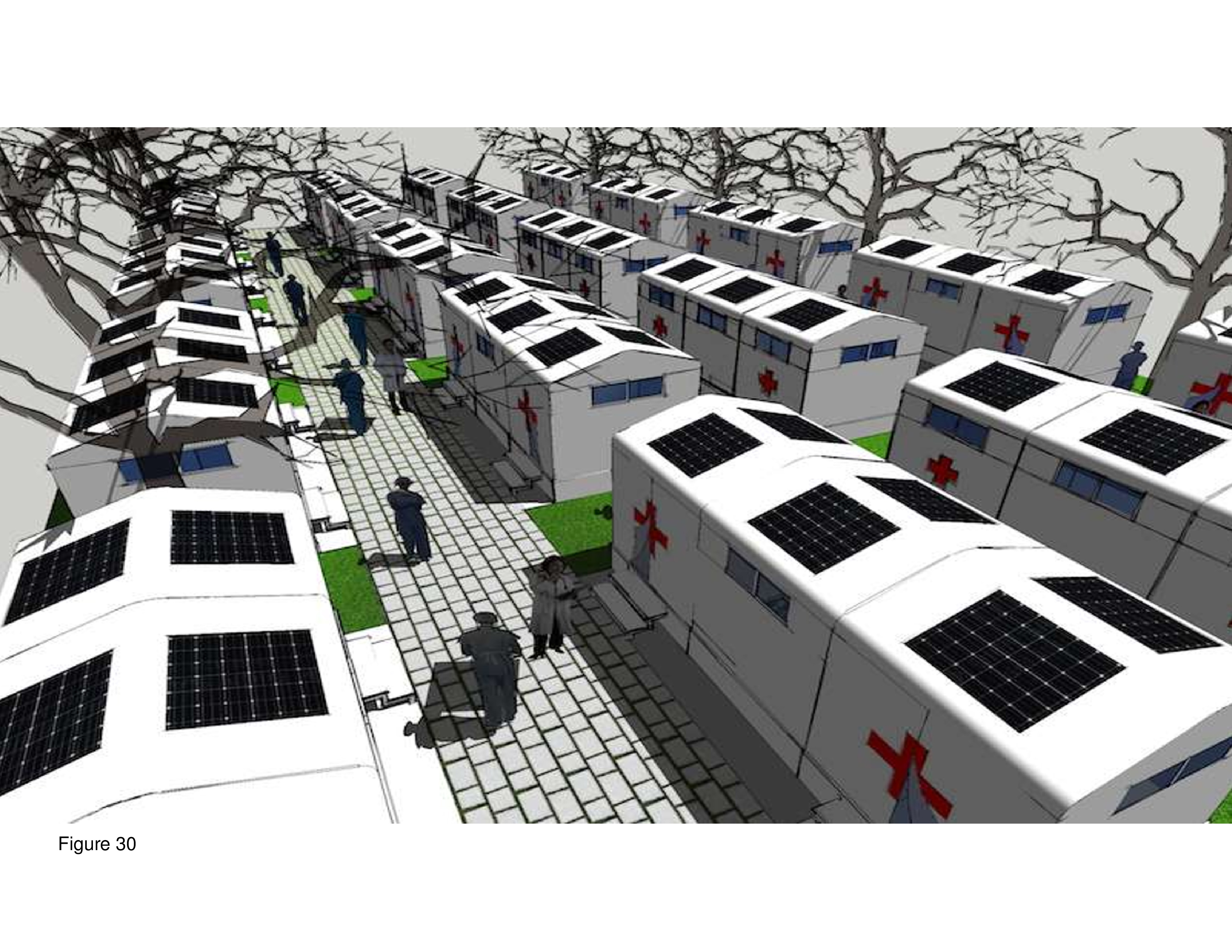
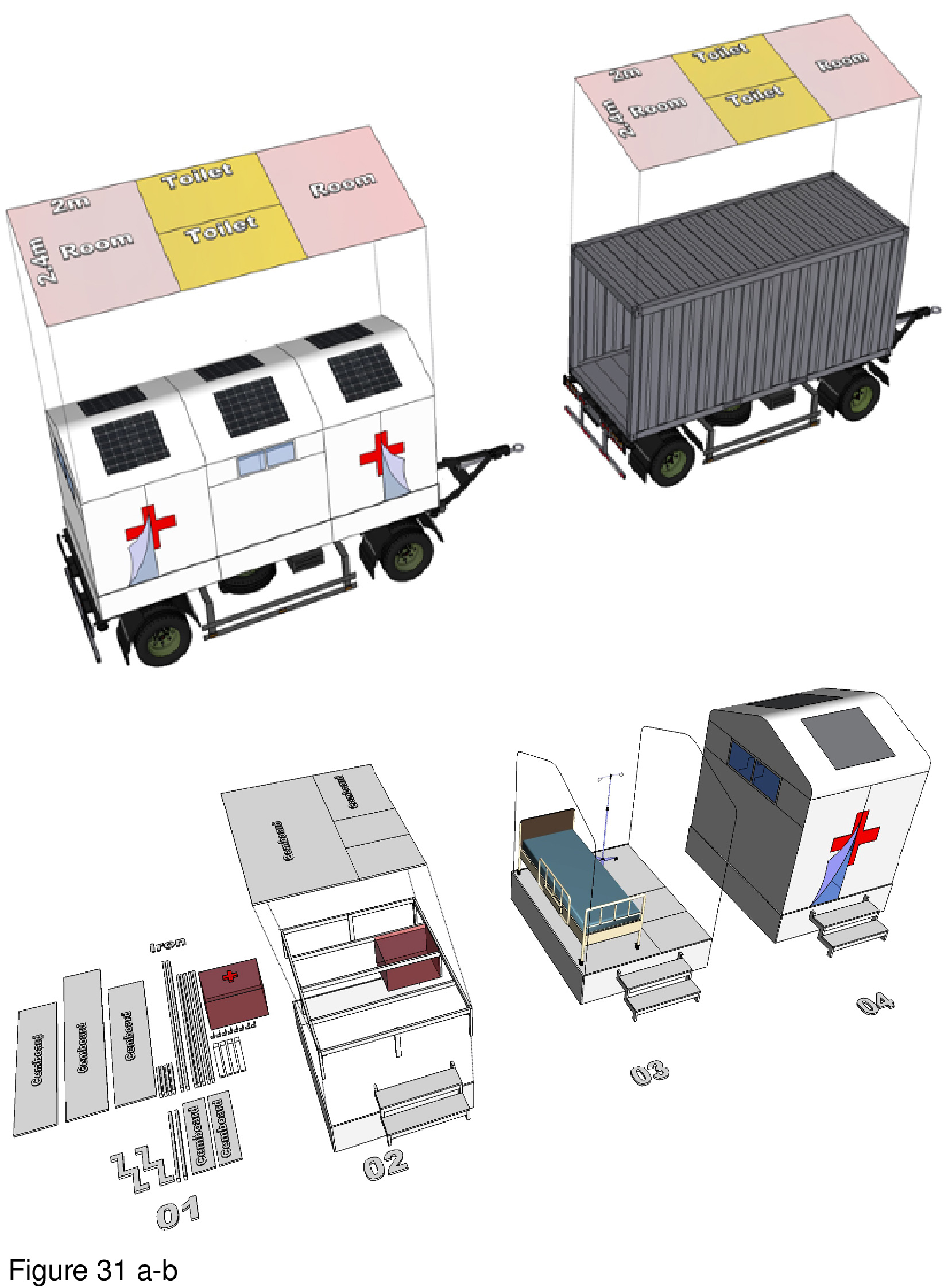
VHL Architecture teamed with Da Nang University’s school of architecture to design this prefabricated surge hospital for COVID-19. Based on a 6sm standard cube module subdivided into three internal zones, the module is 30mm by 60mm and the raised platform is comprised of lightweight concrete panels. Medical supplies and staff workspaces are housed in cube modules designated with the Red Cross logo. Modules are positioned in long rows facing one another, either independently, or interconnected. The interior spaces appear confining, providing little contact with the outside world — especially considering it is designed for outdoor installation. The basic module can be manufactured as a monolithic unit, or as a lift-pack and then assembled onsite. In either case, system componentry is delivered by truck. The installation as shown requires negotiating narrow exterior steps, allowing scant room for egress-ingress error. HVAC and utility infrastructure are installed below the raised platform floor.28 (Figure 30 and Figure 31a-b.)
Micro Treatment Unit
Firm: AT-LARS, Indonesia
This prototype is an intentionally low-cost DIY testing and treatment facility, inspired by standard construction scaffolding. The facility is to be plugged into an existing hospital in need of COVID-19 surge capacity. Transparency is of priority, with exterior and interior wall panels fabricated as opaque off-white polycarbonate panels. Its monochromacy and openness is striking, together with natural-finish wood floor and flat, corrugated steel roof decking. The roof is structurally supported by the steel scaffolding. A minimalist low-tech aesthetic is achieved. Patients are called from the waiting room to a nearby row of windows for the CNST. The test is administered by a specialist sitting on the other side. The facility is open-air and large roof overhangs provide added protection from intense sunlight or sudden downpours. There is no HVAC system and utilities run beneath the floor. The absence of an HVAC system contributes to its low-budget minimalism.29 (Images not shown.)
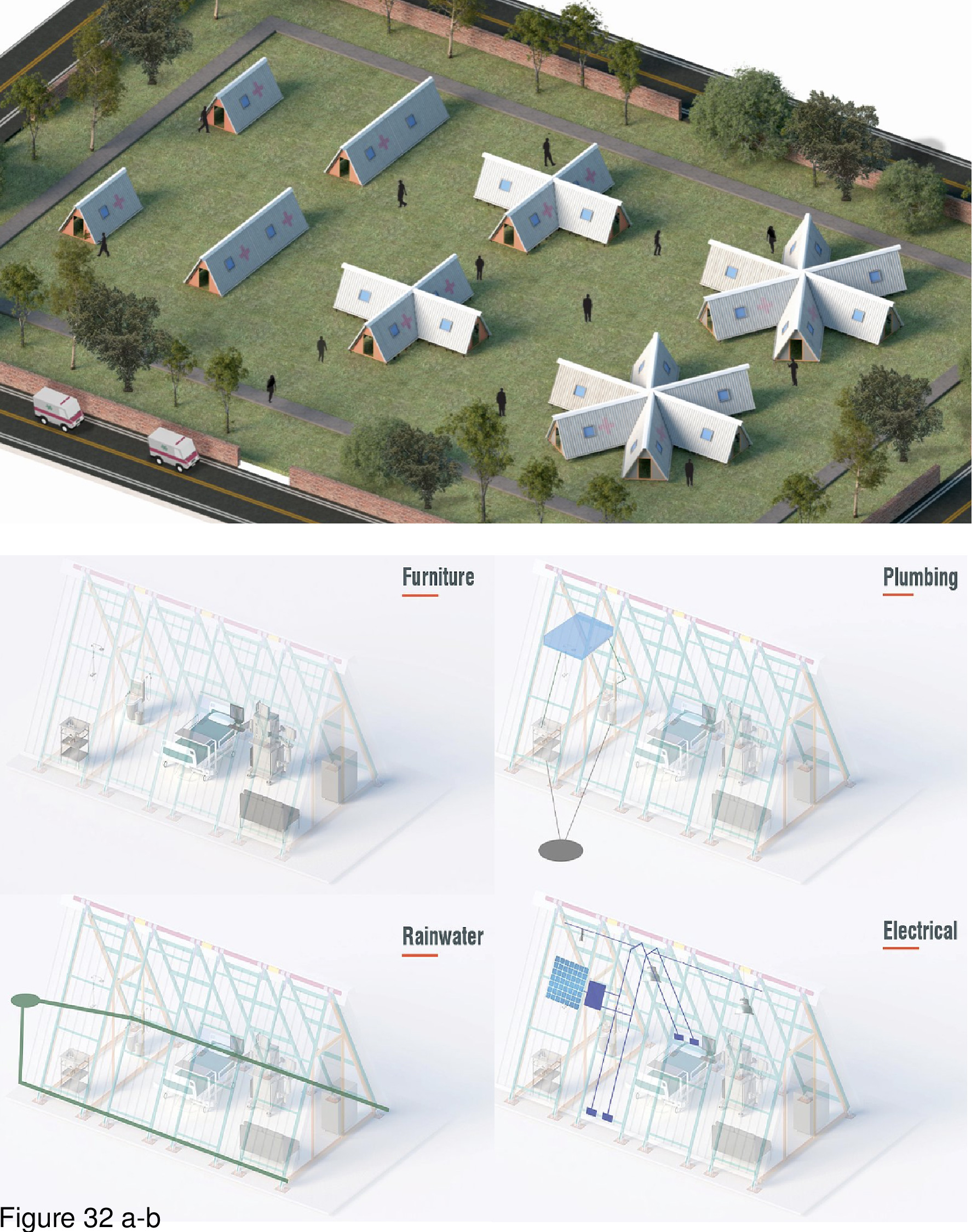
Kaksh
Firm: AGX Architects, Delhi, India
Images: Courtesy AGX Architects
India faced a critical shortage of overflow healthcare facilities throughout the pandemic, and in response, AGX Architects in 2020 proposed a prefab modular A-frame unit. It can serve as an emergency quarantine shelter. This lift-pack can be erected in an afternoon according to its designers. The concept is for units to be installed near hospitals, providing surge capacity for non-ICU level patients that nonetheless require 24/7 medical observation. Units are fabricated in steel and erected directly on a concrete pad or other flat, stable surface. The entry is at one end, and both sloping walls have operable windows. Modules are fabricated in three sizes: 400 square feet (two-bed/toilet), 320 square feet (one-bed/toilet), and 240 square feet (one-bed/toilet). The structural frame is erected first. Next, three-foot-wide full-height metal panels are attached to a lightweight structural frame. The bed is positioned along one of the sloping walls, furnishings and equipment are added. Rainwater drainage, plumbing, HVAC/electrical, and furnishings are provided. The installation shown consists of the three unit types (totalling eight) plus two hexagonal “pinwheels” each consisting of six interlocking modules. Units are naturally ventilated, and HVAC system information was not furnished.30 (Figure 32a-b.)
Huoshenshan Hospital
Agency: Government of China, Wuhan, China
This 1,000-bed COVID-19 field hospital was built in fourteen days near Zhiyn Lake, in Wuhan. A second field hospital, Leishenshan Hospital, was built just as rapidly using the same design and it also opened in February of 2020. The site of the first facility was expediently prepared by a small army of earth movers (shown). The hospital’s foundation consisted of several layers of fibrous matting insulation with interspersed layers of concrete. Up to 7,000 people worked around the clock in three shifts. The design was based on the Xiaotangshan Hospital, a facility built in the suburbs of Beijing in six days during the SARS pandemic in 2003. The hospital at Wuhan was modular and prefabricated, with two levels housing thirty ICUs, nursing and medical support, and multi-bed quarantine units. Each module is 10 metres by 10 metres and houses two beds and all rooms are negatively pressurized. This surge hopsital was staffed by 1,400 medical personnel.31 The Wuhan hospital garnered extensive international media coverage for its extremely rapid construction and massive size. For these reasons it is fair to view this facility as the mother of all specialized COVID-19 facilities built worldwide.32 Despite the magnitude of this government-commissioned engineering achievement, the interior spaces were strikingly bare-bones with its occupants lacking visual contact with the outside. Both Huoshenshan and Leishenshan surge hospitals were closed in April of 2020, when local community transmission rates had subsided significantly. They remain on standby in the event of a resurgence of cases in the region. (Figure 33a-b and Figure 34a-f.)
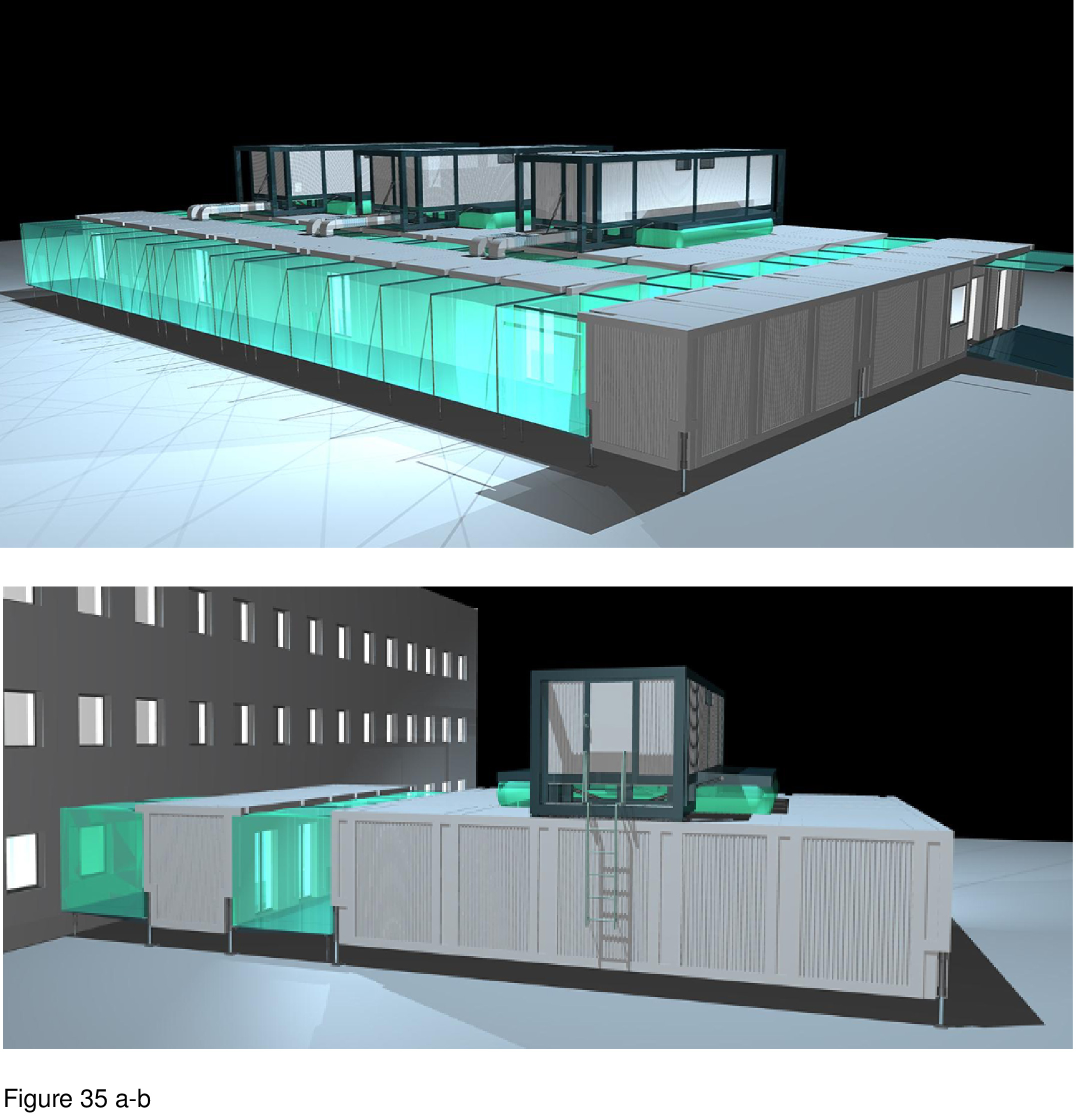
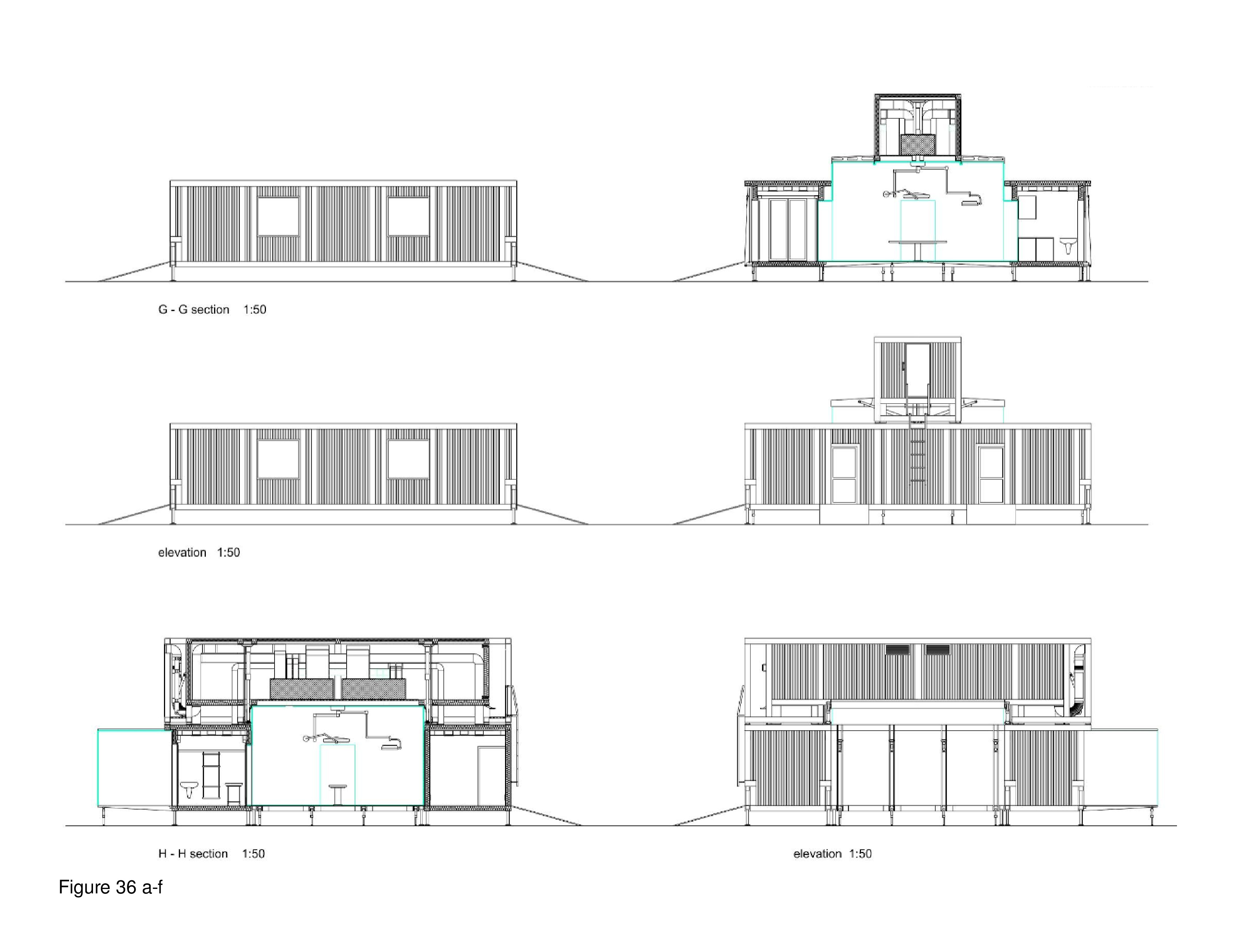
Field Rescue Center
Firm: HAHA Architects Group, Warsaw, Poland
Images: Courtesy HAHA Architects Group
The Field Rescue Center (FRC) prototype is a mobile diagnostic and treatment facility for emergency response including epidemics, pandemics, natural disasters, refugee crises, and humanitarian missions where emergency ICU-surge capacity is required. This one-level facility consists of interlocking TEU-FRC modules close-packed in a grid configuration. HVAC, plumbing, and electrical/IT equipment is housed in roof-mounted modules servicing spaces below. Circulation occurs in translucent perimeter modules with tinted polycarbonate wrap-around panels simultaneously functioning as wall-roof elements; these aqua-tinted paths are visually striking, and a platform-floor supports the installation. This facility can house ICU beds, emergency diagnostic and treatment services, or a combination. The FRC is shown here plugged into an acute care mothership.33 Construction documents are available online as open access documents. (Figure 35a-b and Figure 36a-f.)
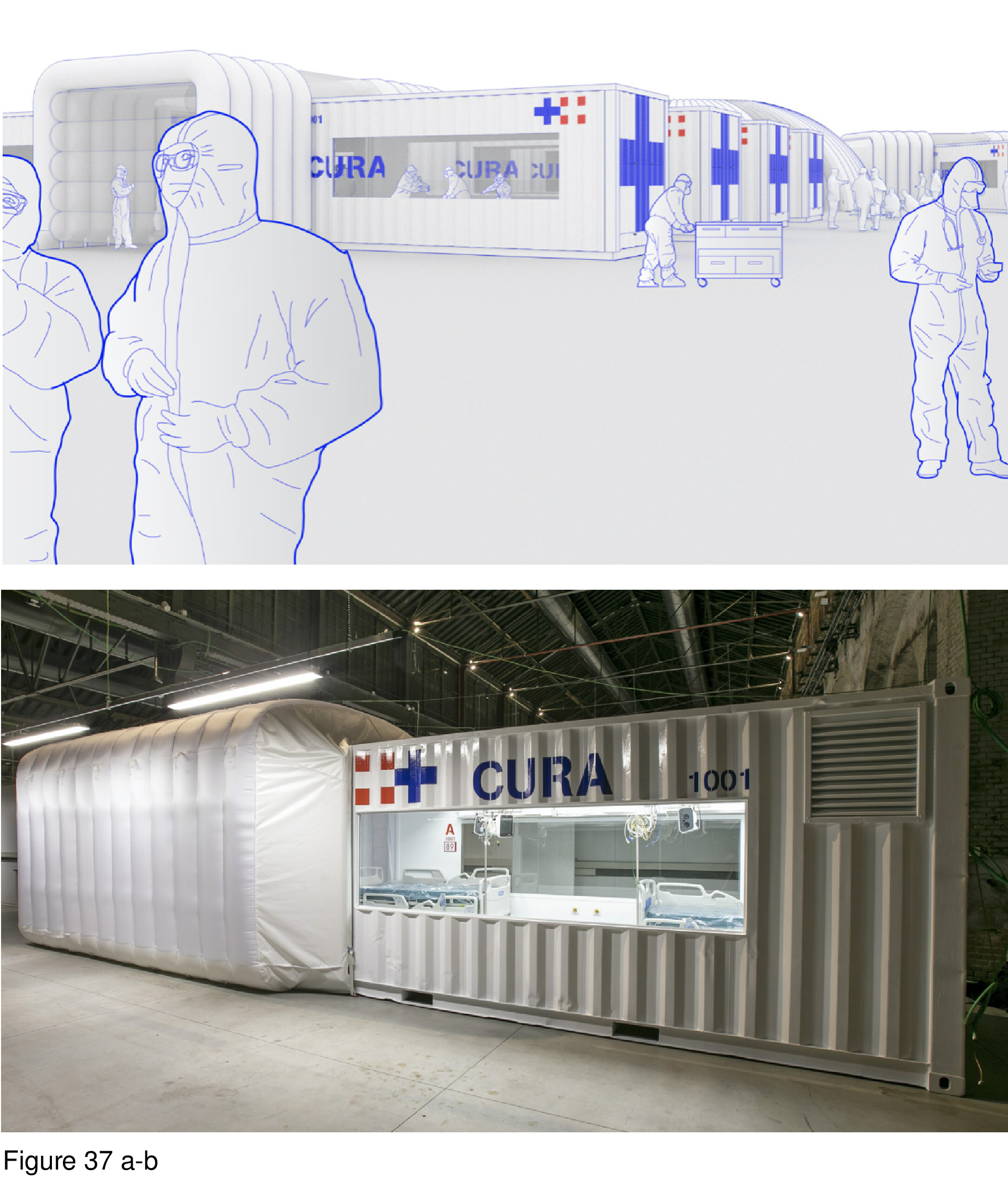
CURA Pod
Firm: CRA—Carlo Ratti Associati with Italo Rota, Turin, Italy
Photos/Images: Courtesy of Max Tomasinelli and CRA
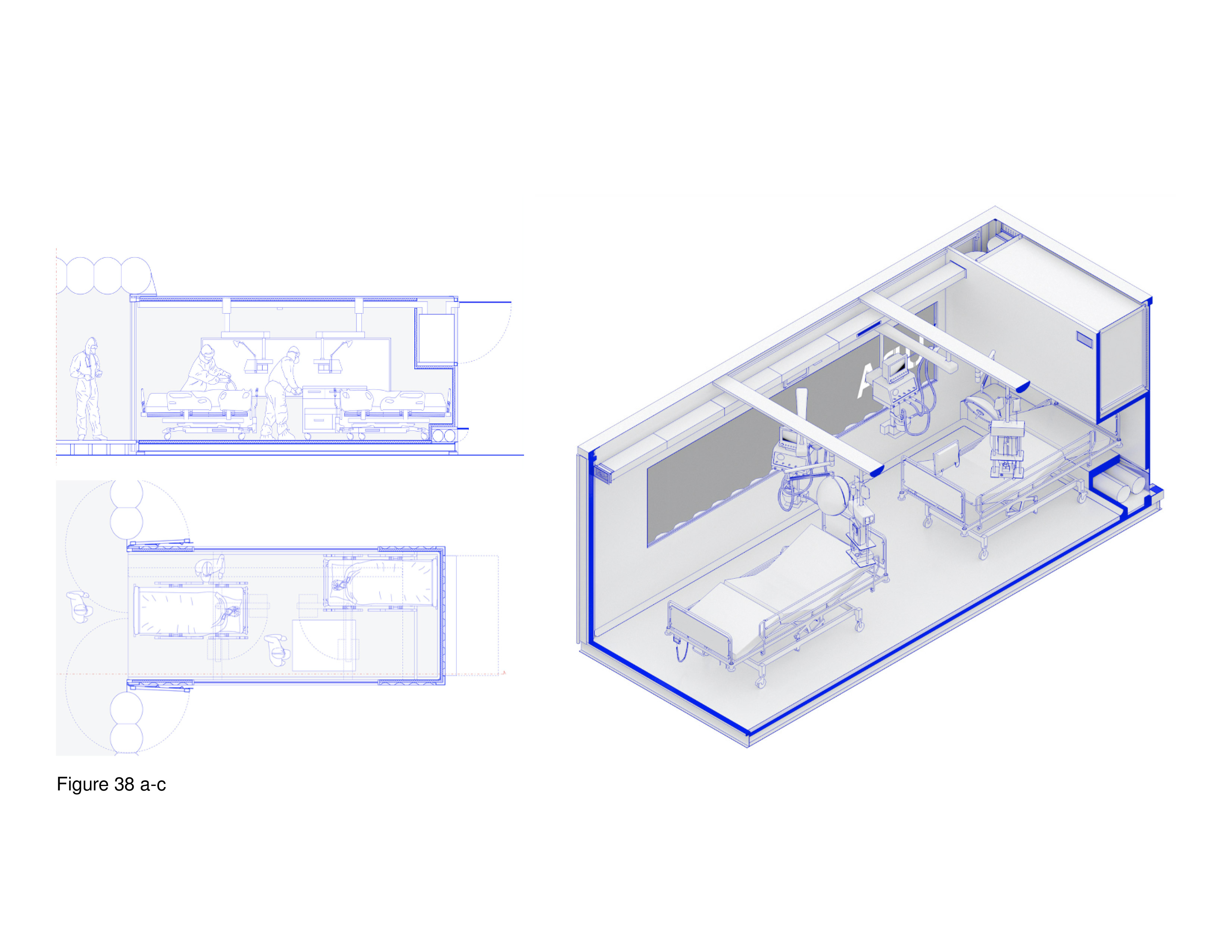
This container-based modular prototype was built at a Turin hospital in March of 2020. Named the Connected Units for Respiratory Ailments (CURA), the first unit was installed as part of a surge field hospital at the Officine Grandi Riparazioni complex in central Turin. Based on a generic 6.1-metre-long intermodal shipping container, each pod houses two beds and required medical equipment. The main design challenge was to ensure that physicians would accept treating COVID-19 patients in a shipping container. Containerization was seen as offering the quickest assembly for ICU-level patient care, in transiting, and in ensuring reliable negative air pressurization — attributes fabric and pneumatic-supported tents could not guarantee, in the architects’ opinion. Specially fitted ozone filters ensure pressurization leaks do not occur. A container can function autonomously or in tandem with a fabric-sheathed circulation spine, allowing for larger-scale installations. Small glass windows are cut into the sides of the container, allowing views out and staff and family to view in. Technical drawings and specifications are online open source documents. At this writing, the CURA Pod is being adapted for fabrication and deployment in Italy and beyond.34 (Figure 37a-b and Figure 38a-c.)
STAAT Mod
Firm: HGA+The Boldt Company, USA
Images: Courtesy HGA.
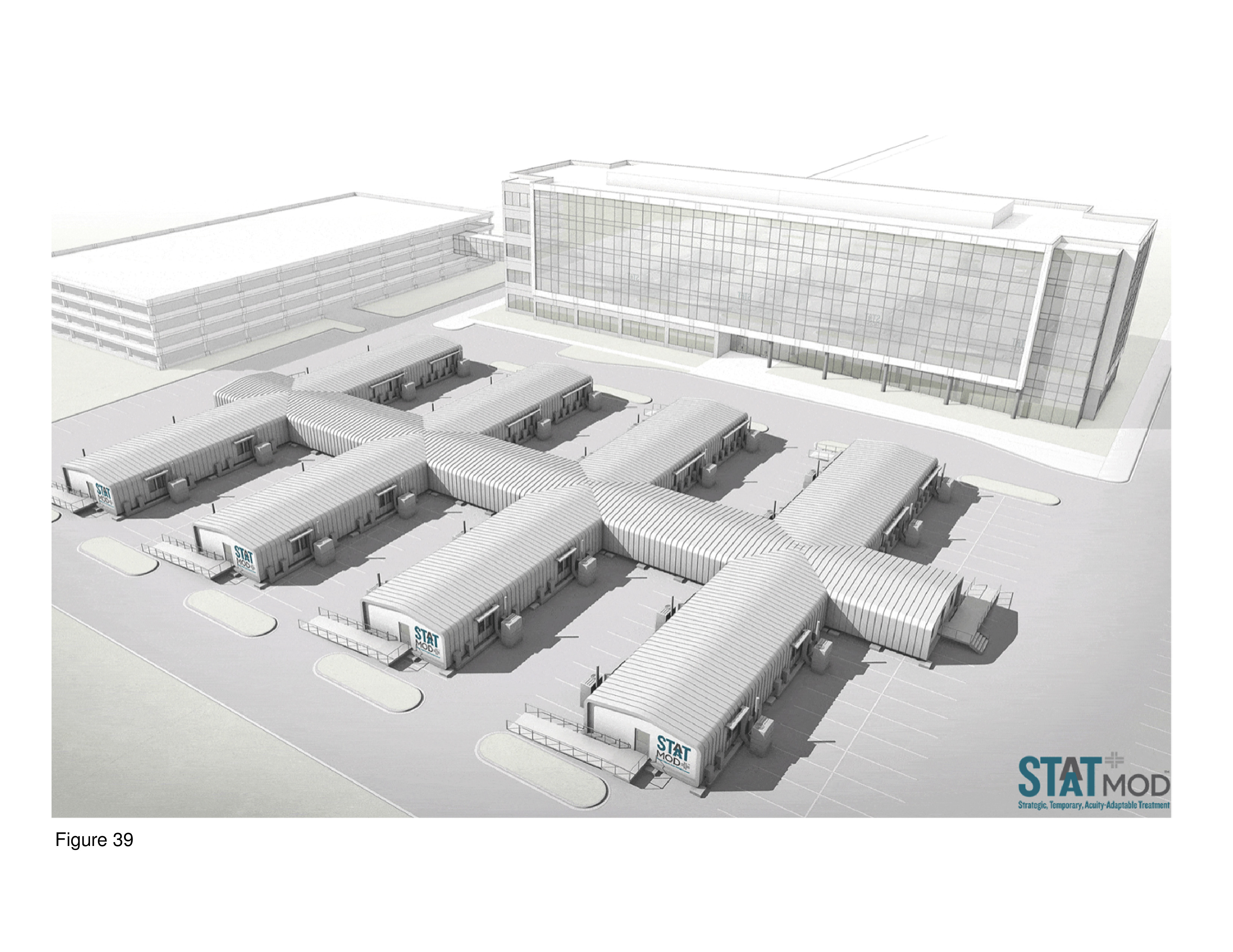
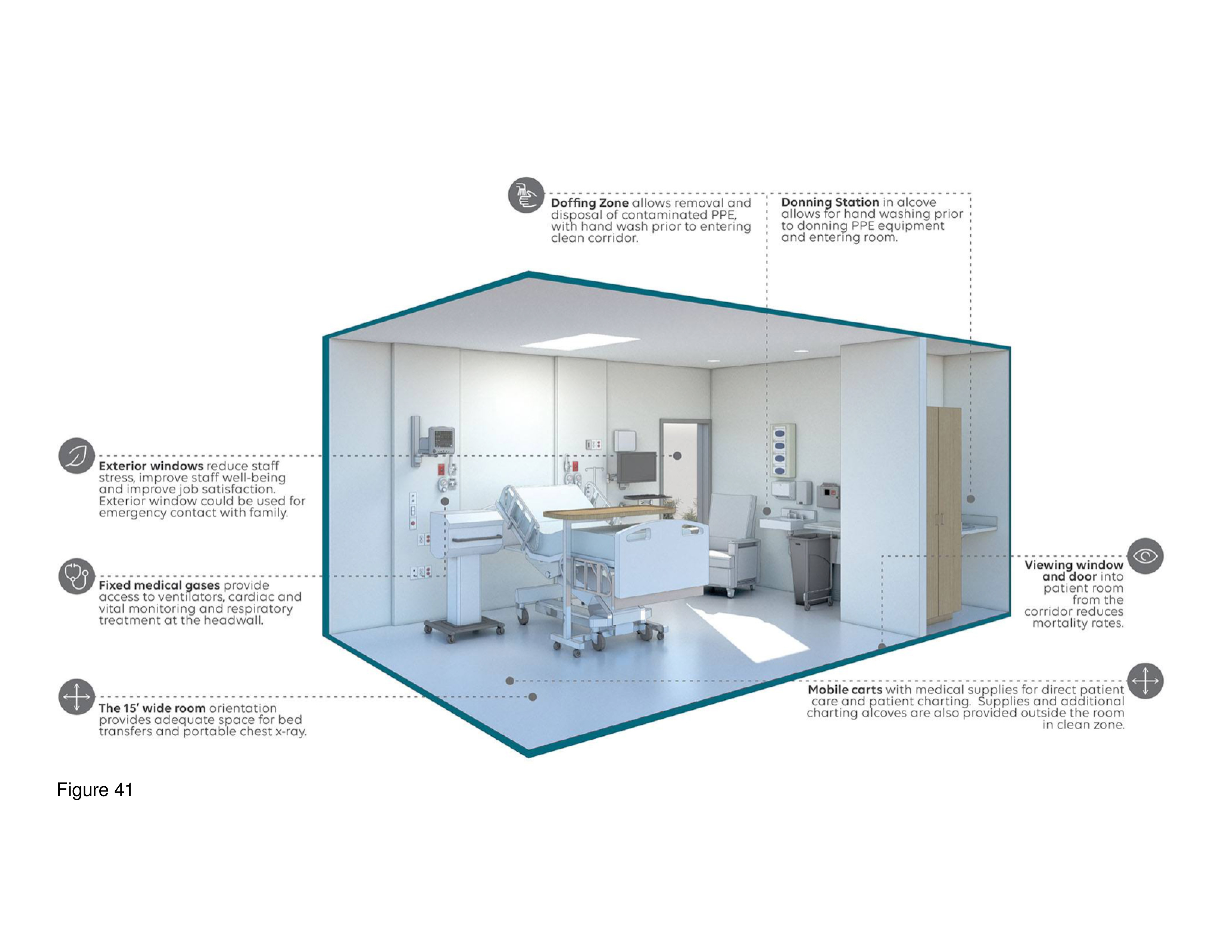
The Strategic, Temporary, Acuity-Adaptable Treatment (STAAT Mod) prefab modular system was designed by HGA and constructed by the Boldt Company for COVID-19 patient care. It is designed for installation indoors or as a freestanding outdoor medical unit adjacent to an acute care mothership. Unit variations consist of a two-room module for interior installations; an eight-bed ICU module consisting of four 20-bed modules plugged into an existing hospital; and a 12-bed module with negatively pressurized open bays (four 3-bed open bays) with a central support spine. The system allows for modules to be added or subtracted without compromising functionality. Modules are 12.5 by 40 feet by 10 feet in height. The system was piloted using stationary, virtual reality simulation walk-throughs with caregivers including nurses, infection control specialists, and LEAN system engineers. The STAAT Mod system’s full footprint is reminiscent of the spine-and-finger configurations typical of 19th to early 20th century Nightingale hospitals. This patient housing module has small windows, however, in contrast to the large windows of the classic Nightingale hospitals.35 (Figure 39, Figure 40a-e and Figure 41.)
Monash Health RESUS Facility
Firm: SPACECUBE, Melbourne, Australia
Photos: Courtesy of Stu Morley and Chris Murray.
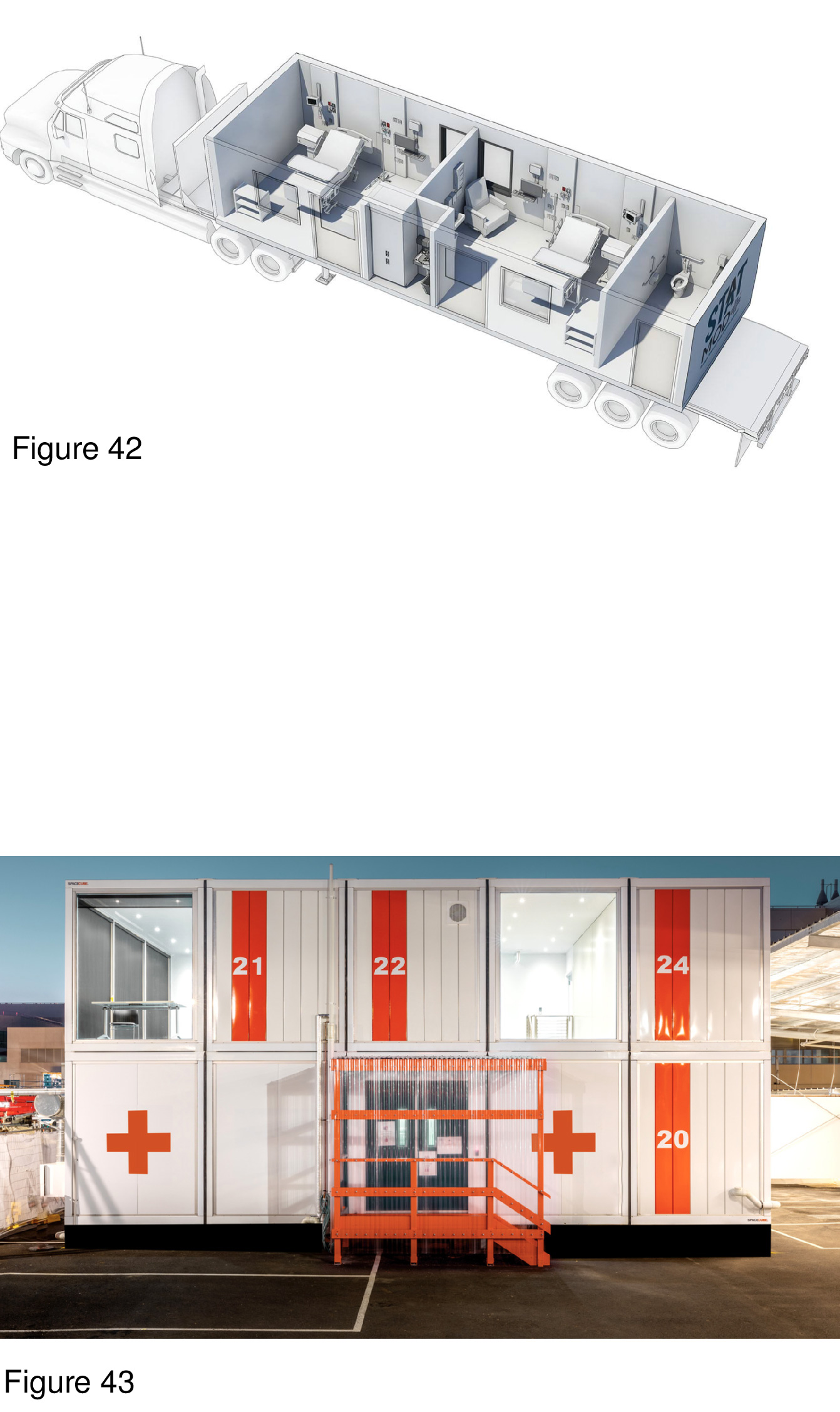
Australia’s first COVID-19 RESUS ICU-surge facility was fabricated in three weeks’ time based on a design developed by SPACECUBE. It was installed next to Monash Medical Centre’s emergency department in 15 hours. Erilyan Construction was commissioned to produce the internal fit-out for this system’s medical equipment. This portable field hospital was commissioned to provide surge capacity while the acute care mothership’s emergency department was undergoing renovation and expansion during the pandemic. The installation shown here consists of 25 lift-pack modules, totaling 360sm on two levels, housing six negative-pressure ICU beds, nurse’s station, medication room, and support spaces including a staff break room. Isolation rooms feature sliding glass doors, with exterior windows affording full views to the outside (a rarity). The architectural vocabularly is Miesian-inspired and its interior spaces are bright and well-appointed — not unlike a conventional hospital’s ICU. The Red Cross logo is set against the white exterior of the containers.36 (Figure 42, Figure 43 and Figure 44a-f.)
University of Toronto Architecture + Health Graduate Design Studio
Project 2: COVID-19 surge field hospital
The second studio project in the fall of 2020 (seven weeks in duration) consisted of the programming and design of a Type 4, 24/7 surge capacity hospital, designed as a lift-pack system, a hybrid lift-pack/containerized system, or a containerized system. The brief called for a modular, prefab prototype in a 50-bed (Phase 1) and also a 100-bed (Phase 2) footprint, installed adjacent to an acute care mothership. Each student team selected four installation sites: a Canadian hospital’s campus plus three additional sites on the grounds of hospitals in other nations. Diagnostic and treatment support is to be provided by the mothership, i.e. MRI, surgery, nutritional services, counseling, administration, materials management, security, housekeeping and central laundry. Finally, as in Project 1, the brief called for incorporating salutogenic and biophilic principles and design features in the design response, i.e. windowed rooms, and indoor surrogate representations of nature. This, in accord with attention restoration theory’s premise that psychologically meaningful engagement with nature can function as a positive distraction during hospitalization. Four Project 2 proposals are presented here:
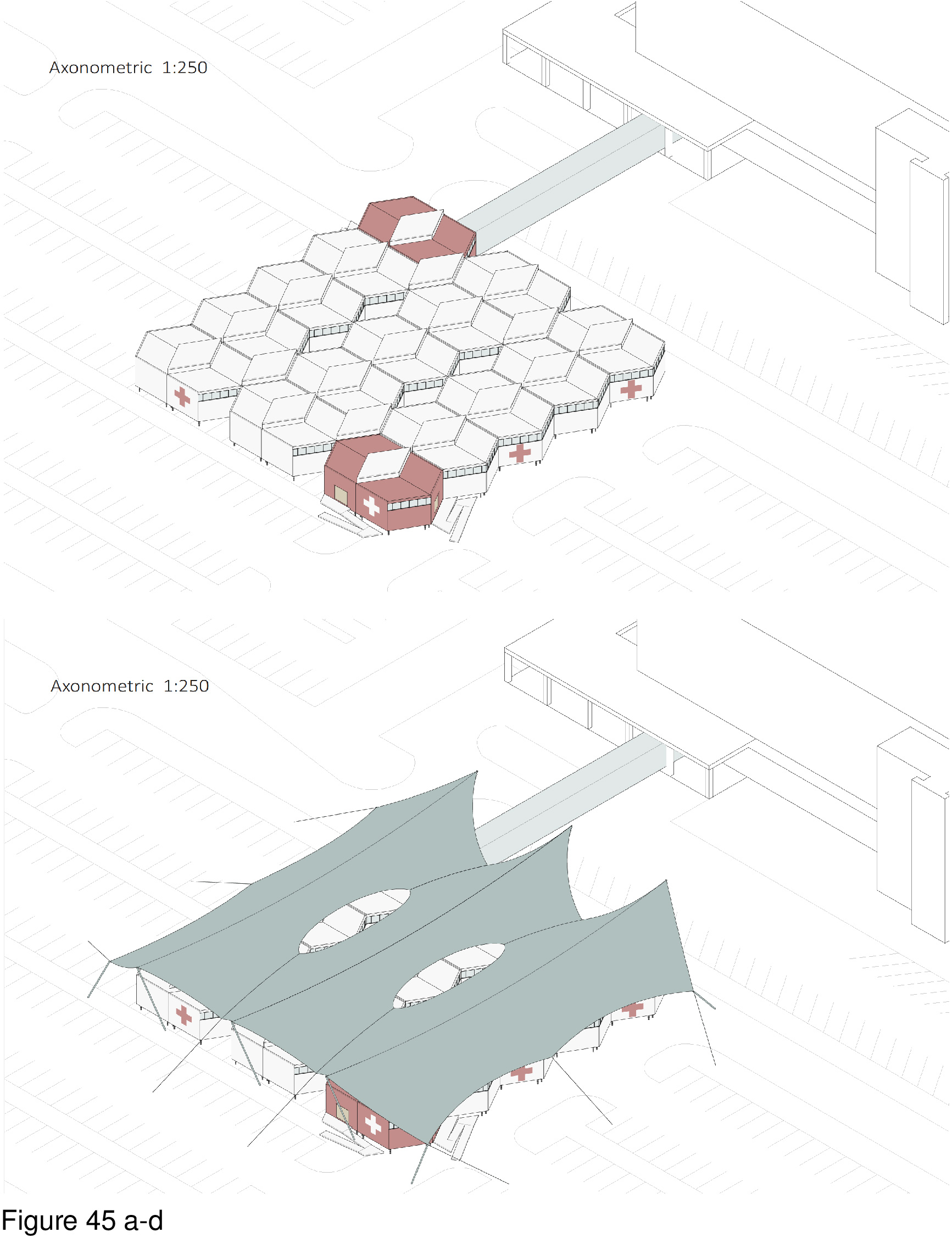
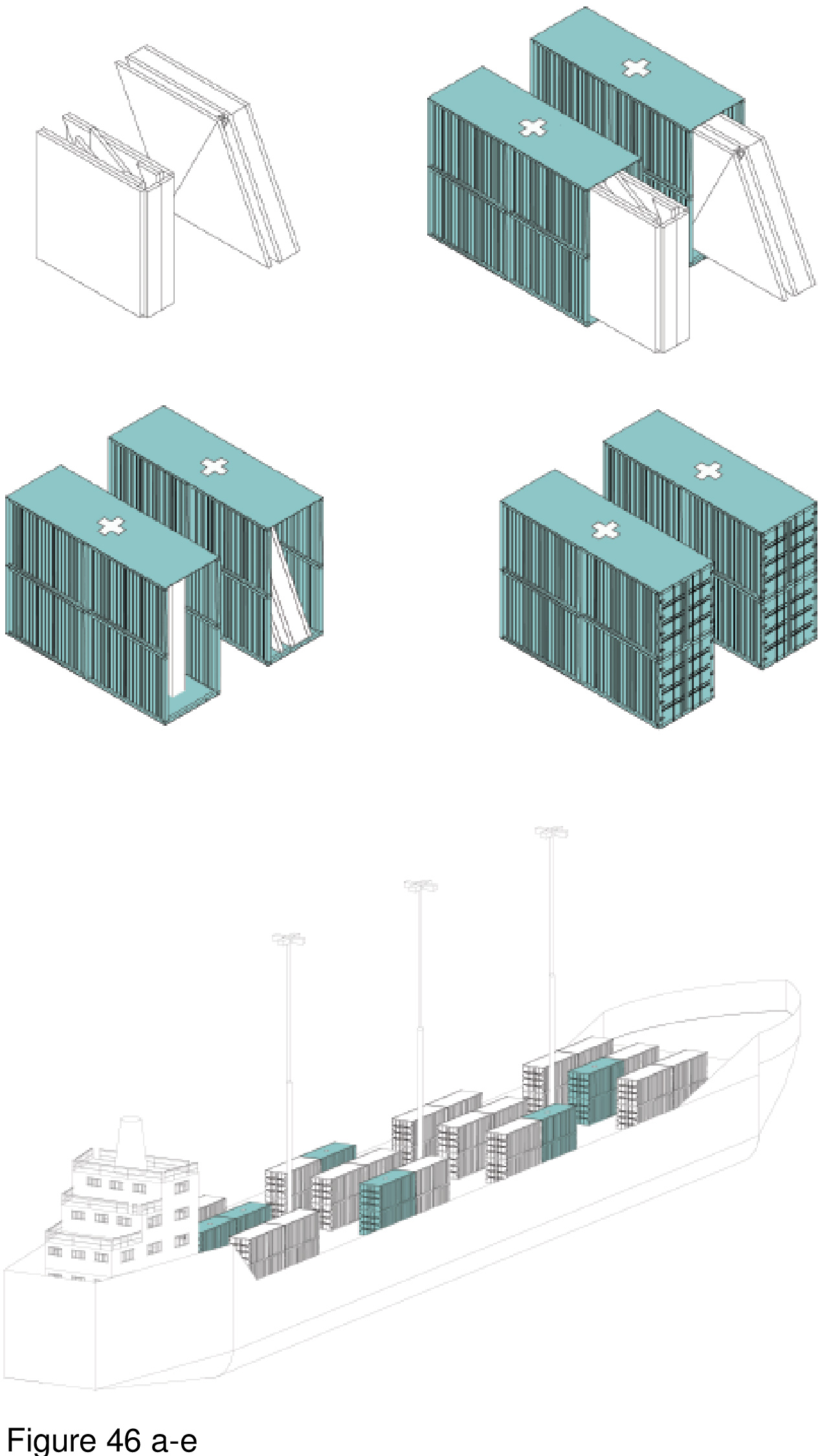
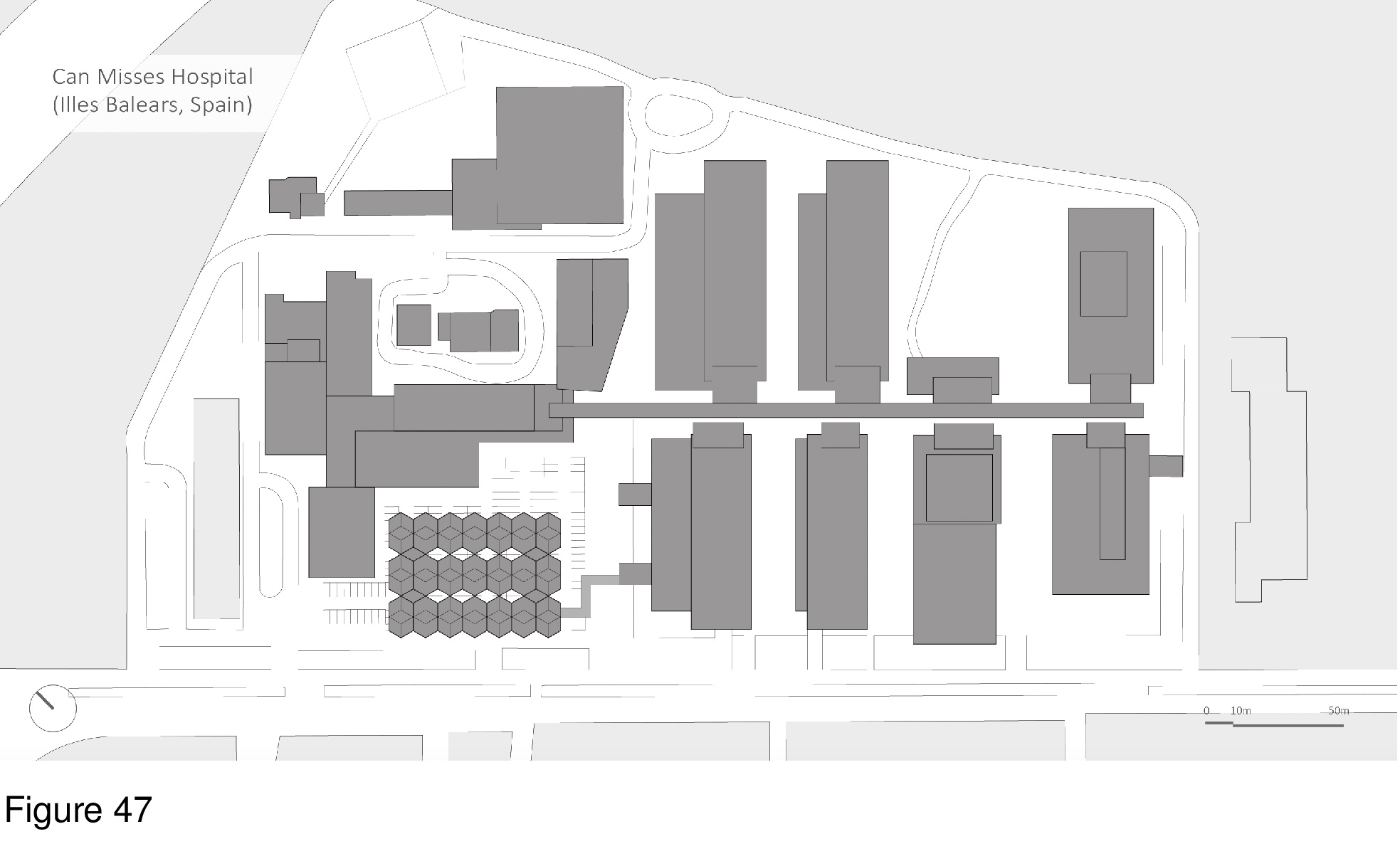
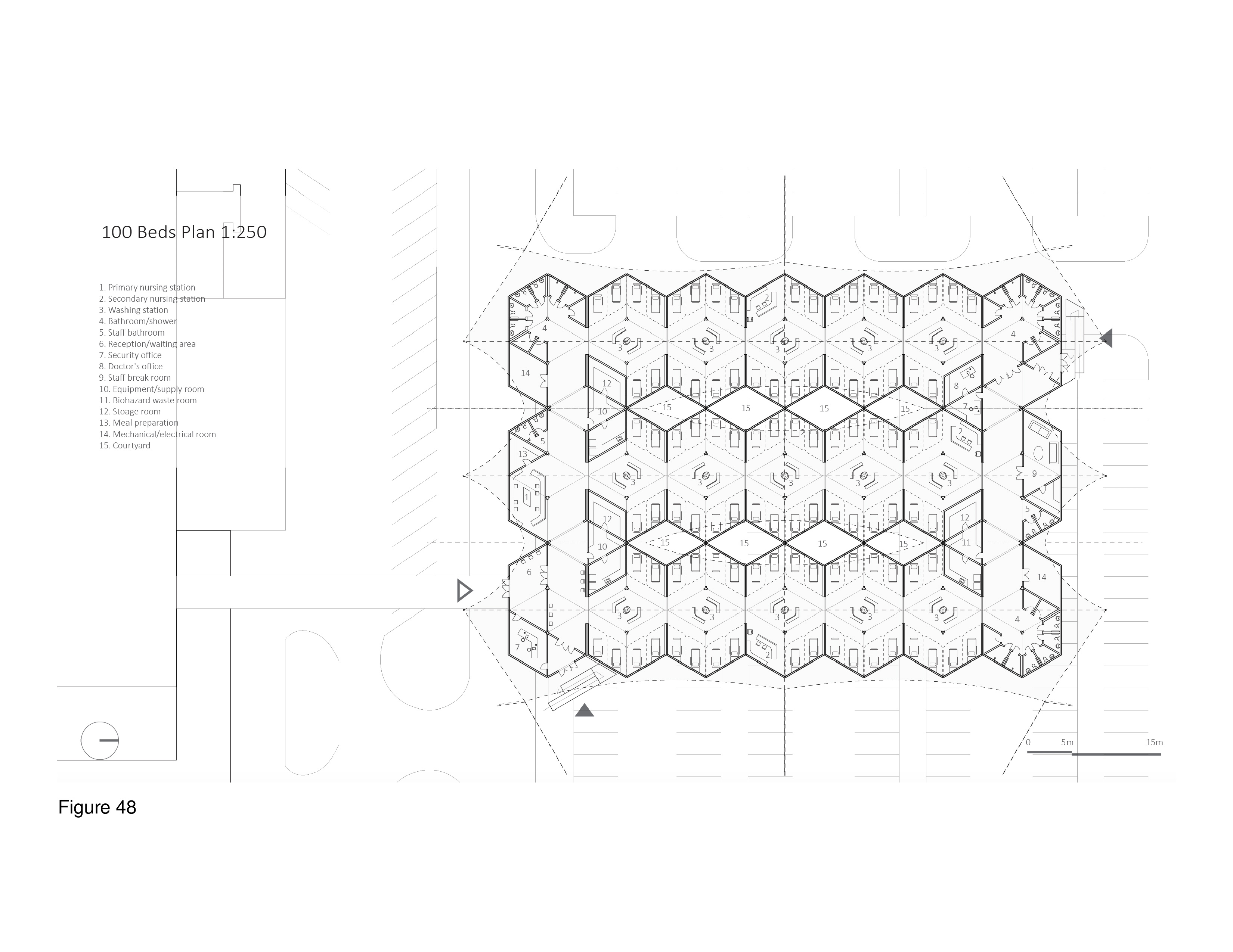
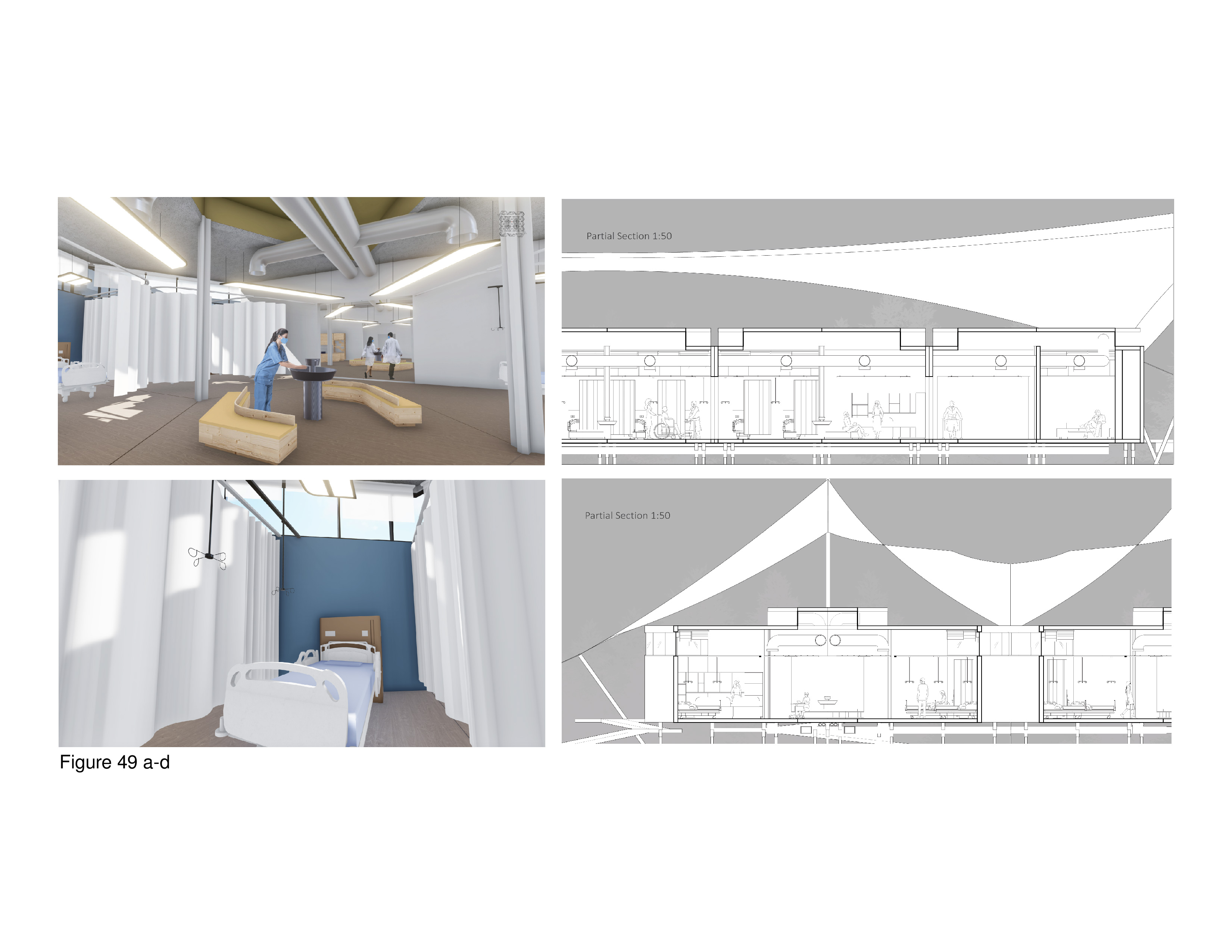
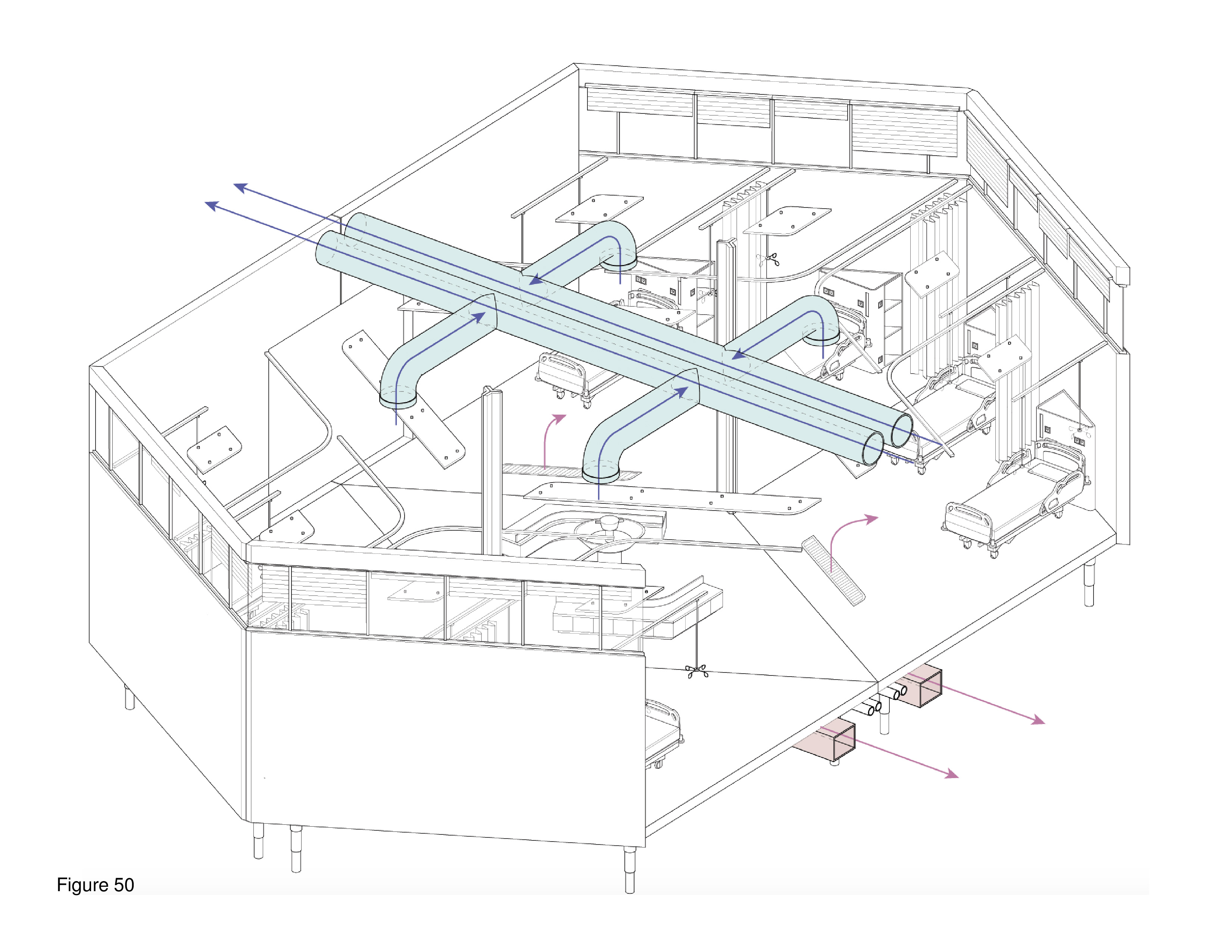
COVID-19 Micro-Courtyard Hospital
Zohar Nekouian Fathi and Yijie Dai
This system is deployable with an optional, cable-supported double-curvature fabric roof. The canopy functions as a sunscreen and to deflect excessive snowloads. The MCH is designed for use in hot, humid regions and in temperate regions. The main arrival point is colour-differentiated, as is the corner module that is connected to the mothership. Modules are transited in containers via ship, plane, rail, and/or truck. A 100-bed installation is shown here on the grounds of the Can Misses Hospital in Illes Balears, Spain. The patient housing modules house four to eight beds each in a semi-open plan, with a series of eight micro-courtyards situated in-between. These exterior spaces, together with clerestories, transmit natural daylight to the interior, are a source of natural ventilation (as appropriate), views out, simultaneously serving as anchor locations for the optional tension-cable supported roof’s lightweight mast-columns. Patient beds are rotated 30 degrees off-grid with the resulting triangulated headwall housing required medical support and storage space. A hand sanitizing station is provided at the centre of each four-to-eight-bed patient care module. Support functions are housed in perimeter modules on opposing edges of the facility, including nurses’ stations, washroom/shower units, staff breakrooms, arrival/intake/waiting areas, consult rooms, medical records, materials management, and general workspace. (Figure 45a-b, Figure 46a-e, Figure 47, Figure 48, Figure 49a-d and Figure 50.)
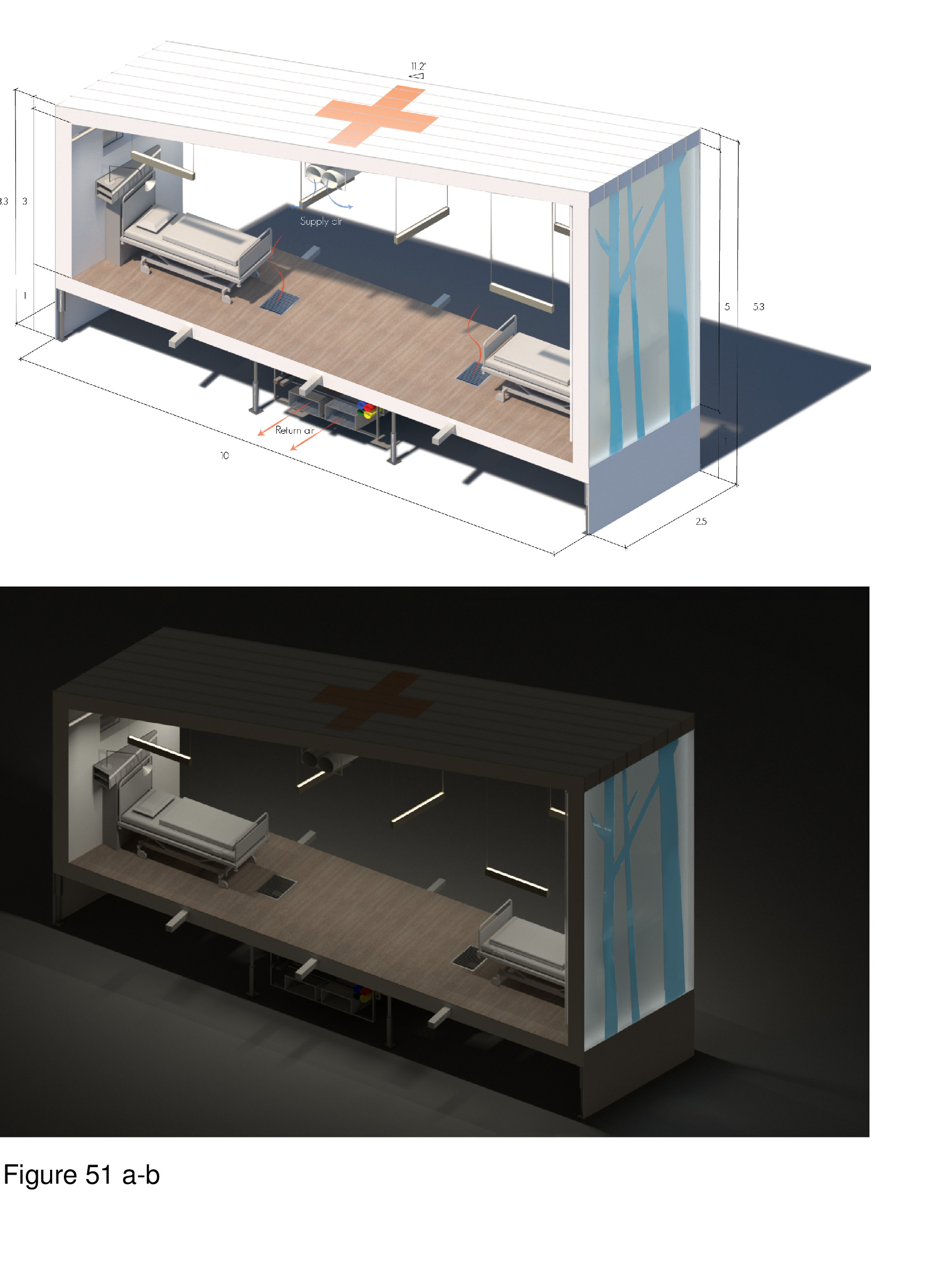
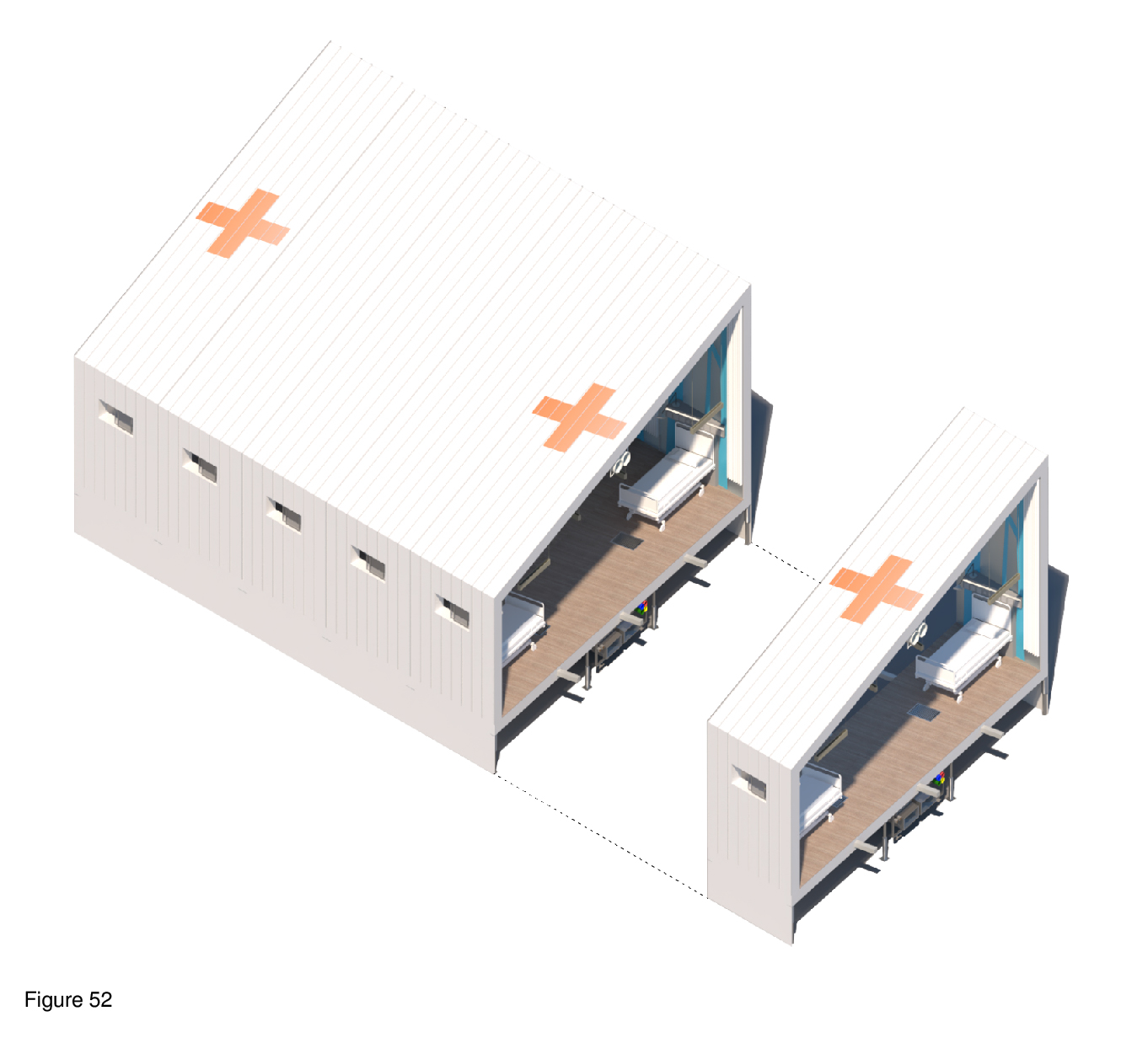
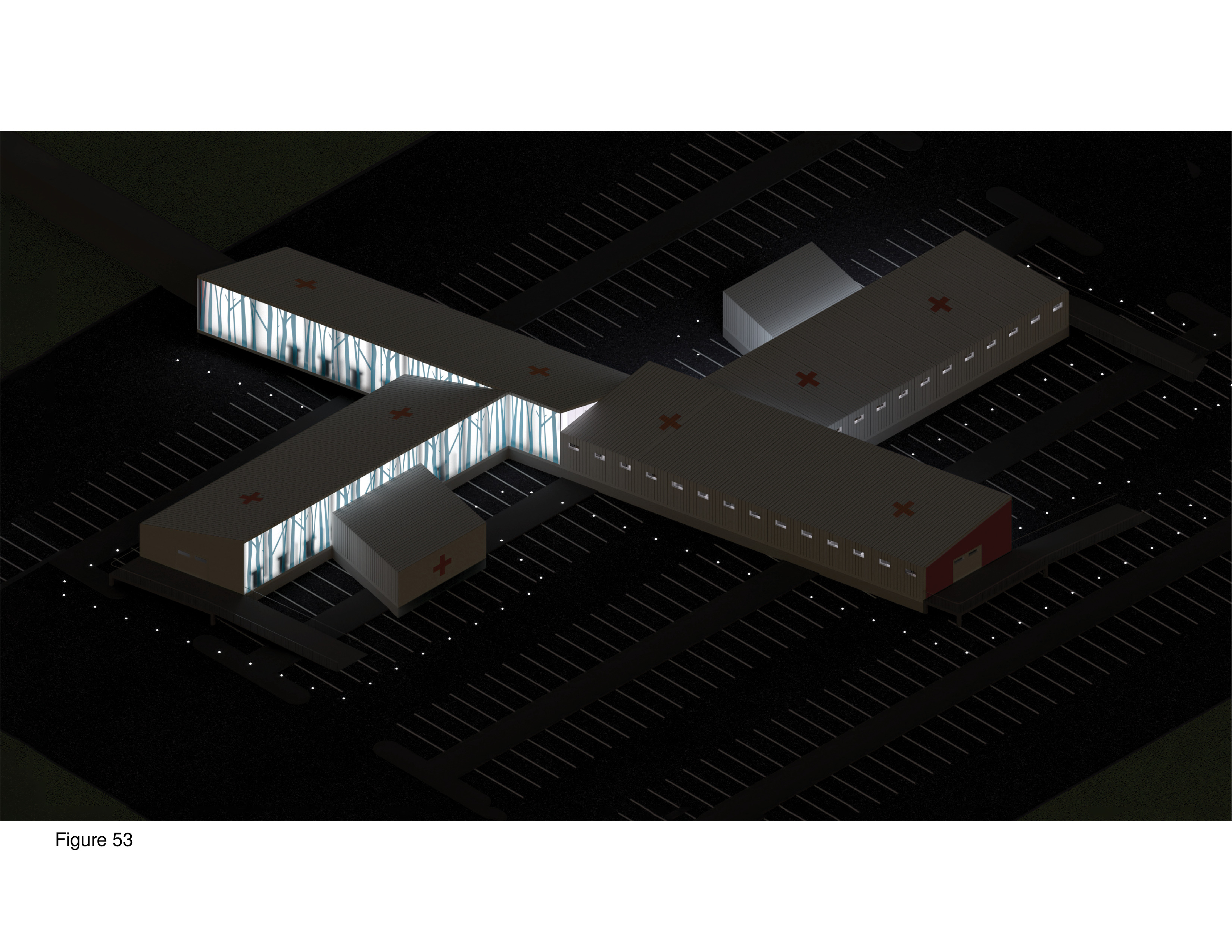
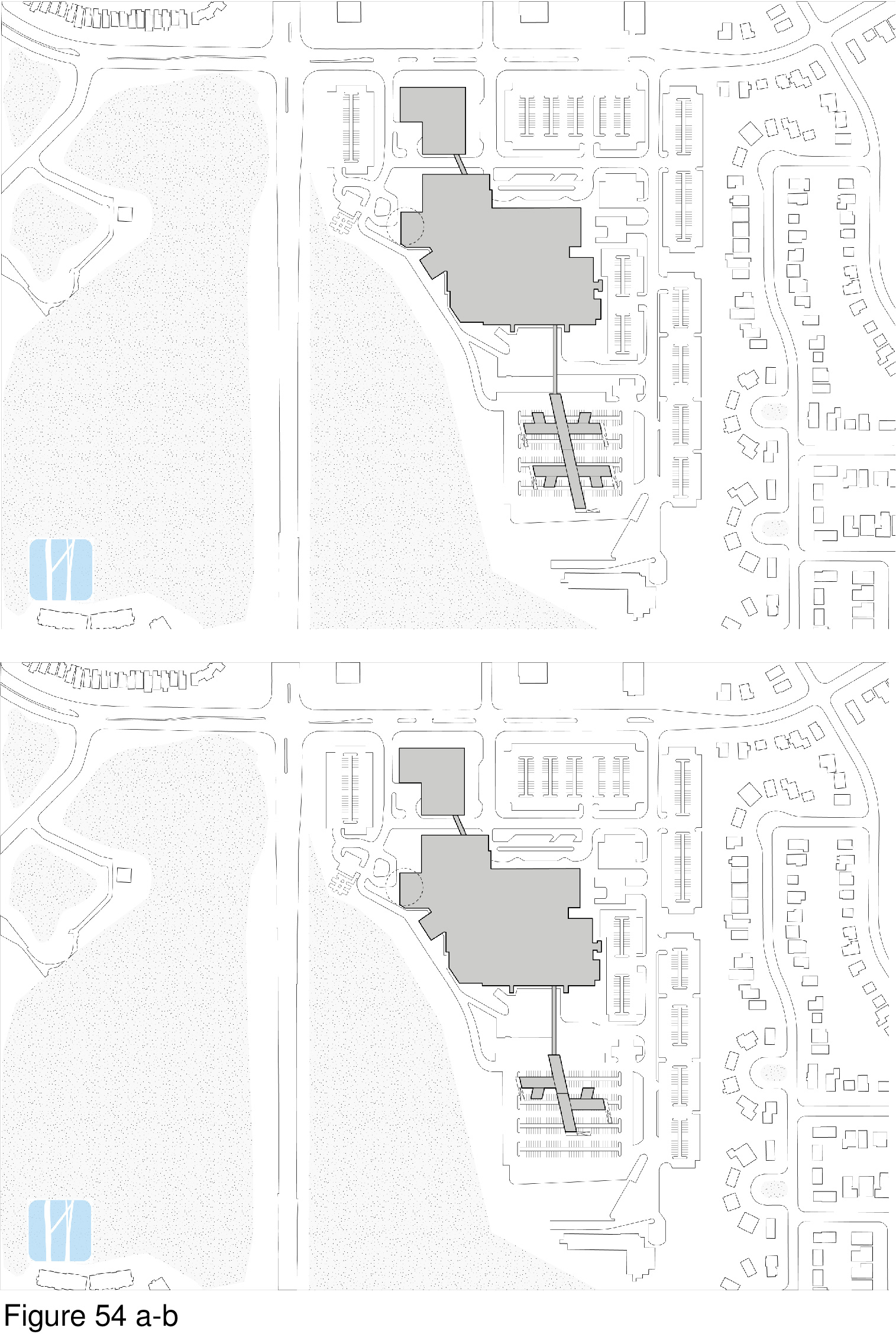
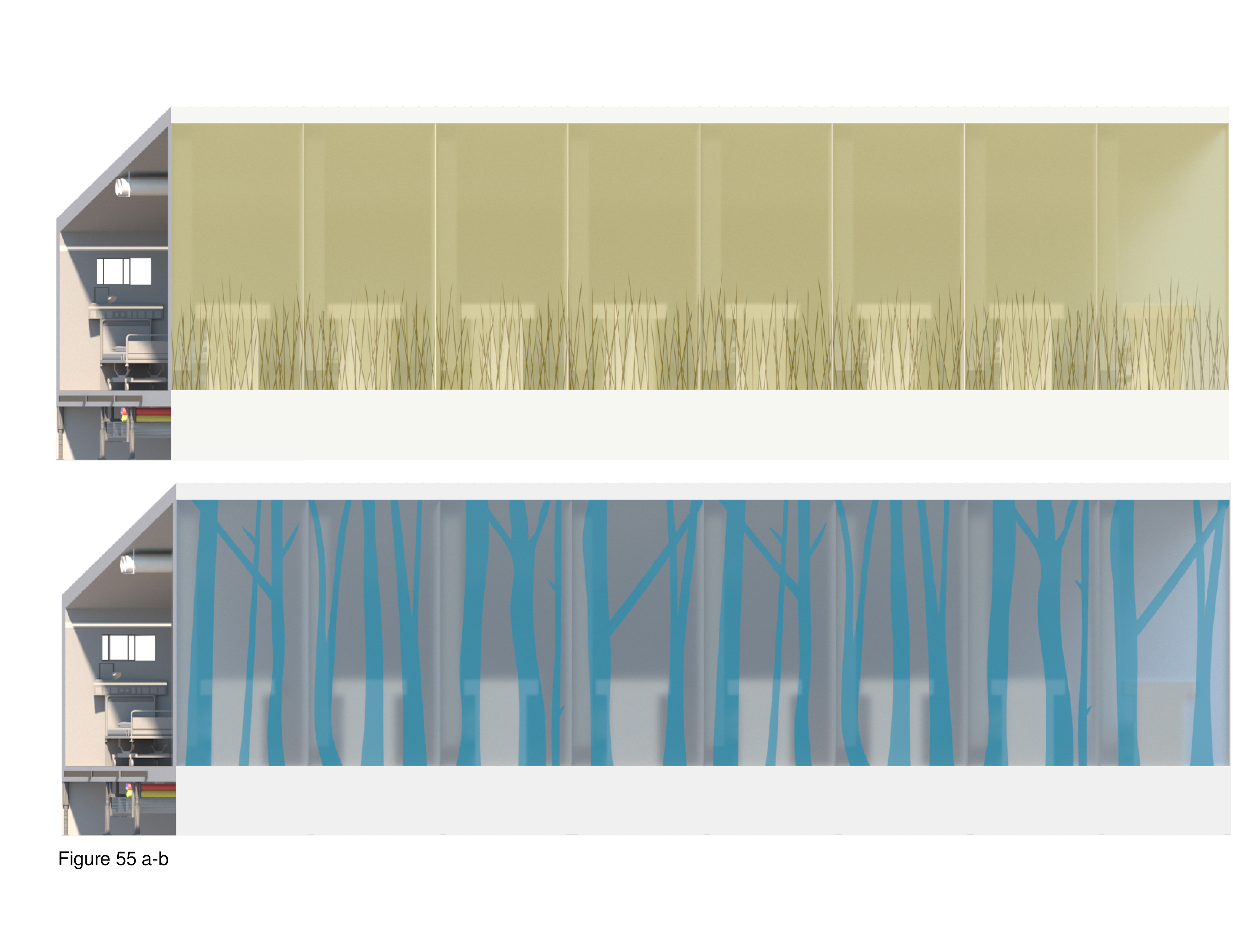
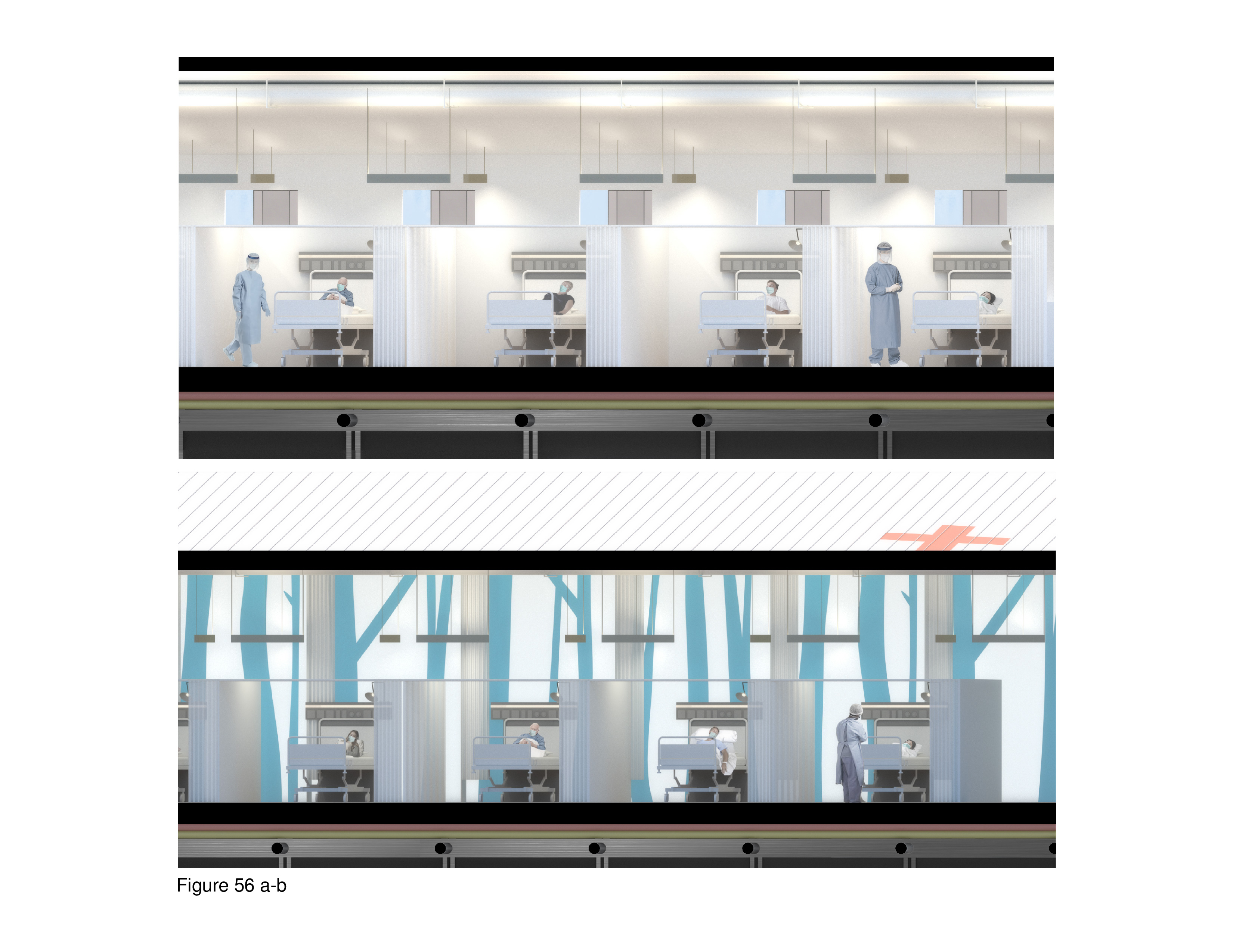
COVID-19 Biophilia Hospital
Bronte Morris-Poolman and Damian Kercz
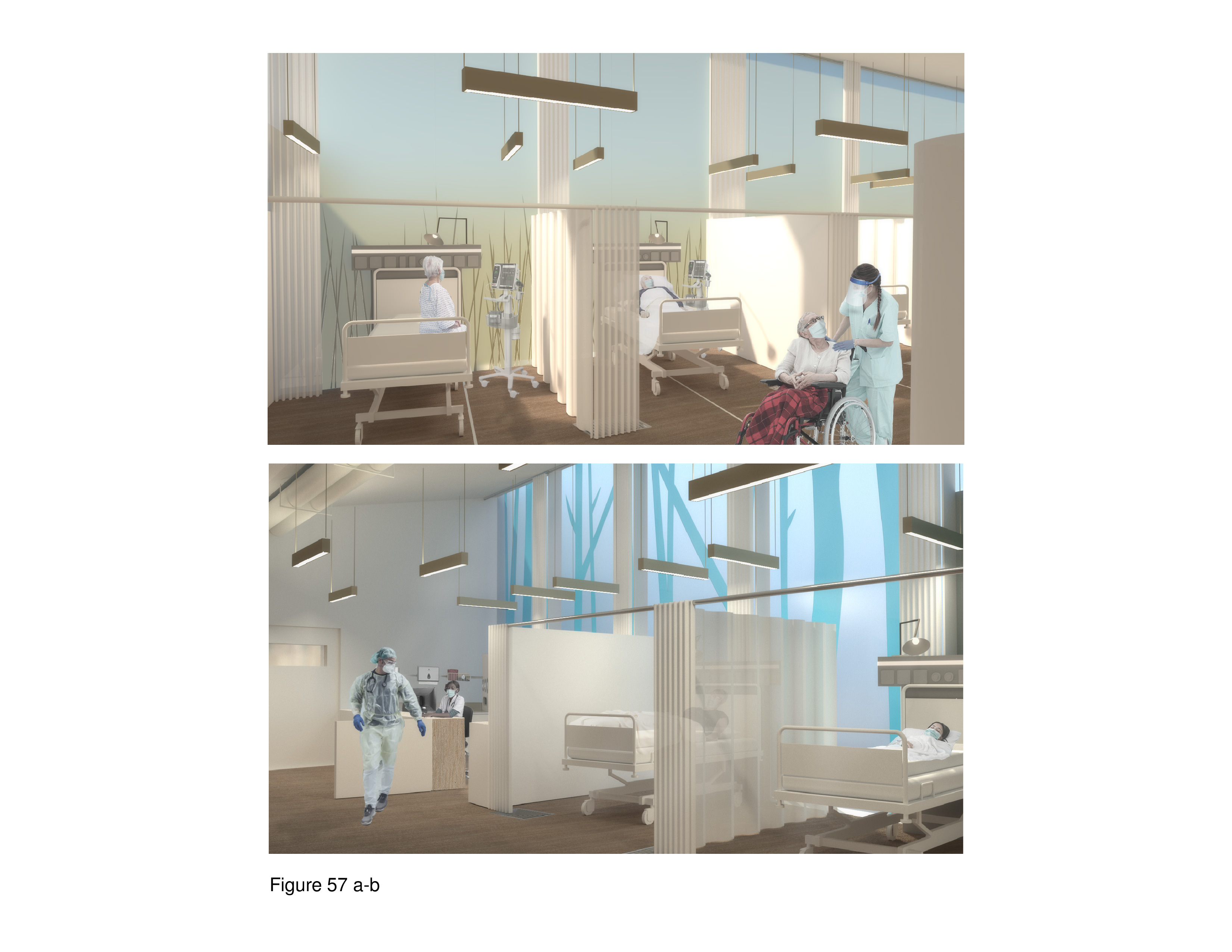
This proposal flat-out rejects mainstream containerized field hospital precursors for their lack of salutogenic and biophilic design amenity. The design intent is to incorporate the therapeutic affordances of natural daylight, views, and interior nature representations as surrogates. By bringing the therapeutic affordances to be found in nature directly into the healing environment, it is assumed that the patient can be more quickly stabilized, and begin the recovery process. The basic module is a lift-up/lift-pack integrated wall-floor-ceiling unit. This module is shipped flat-pack to the site and is hoisted up by crane and then locked into place, side by side, in an iterative manner. This process forms linear wings. Washroom/shower units, medications, materials management, medical equipment, and staff workspaces are housed in plug-in modules that are attached to these wings. The wings house the main entry, intake/registration/waiting, nursing stations and patient care zones. Ceilings slope from six meters to four meters in height. The high wall features translucent polycarbonate panels depicting imprinted images of nature/landscapes. Panels variously depict grassland and forest scenes while transmitting natural daylight to the interior. Patient beds are separated by privacy pull curtains. Negative air pressurization is provided from ducts suspended from the ceiling and exhausted through floor vents. A 100-bed installation at a Toronto-area medical centre is shown here, with its umbilical cord linked to the acute care mothership. (Figure 51a-b, Figure 52, Figure 53, Figure 54a-b, Figure 55a-b, Figure 56a-b and Figure 57a-b.)
COVID-19 Snow Crystal Hospital
Emily Moore and Jiawen Lin
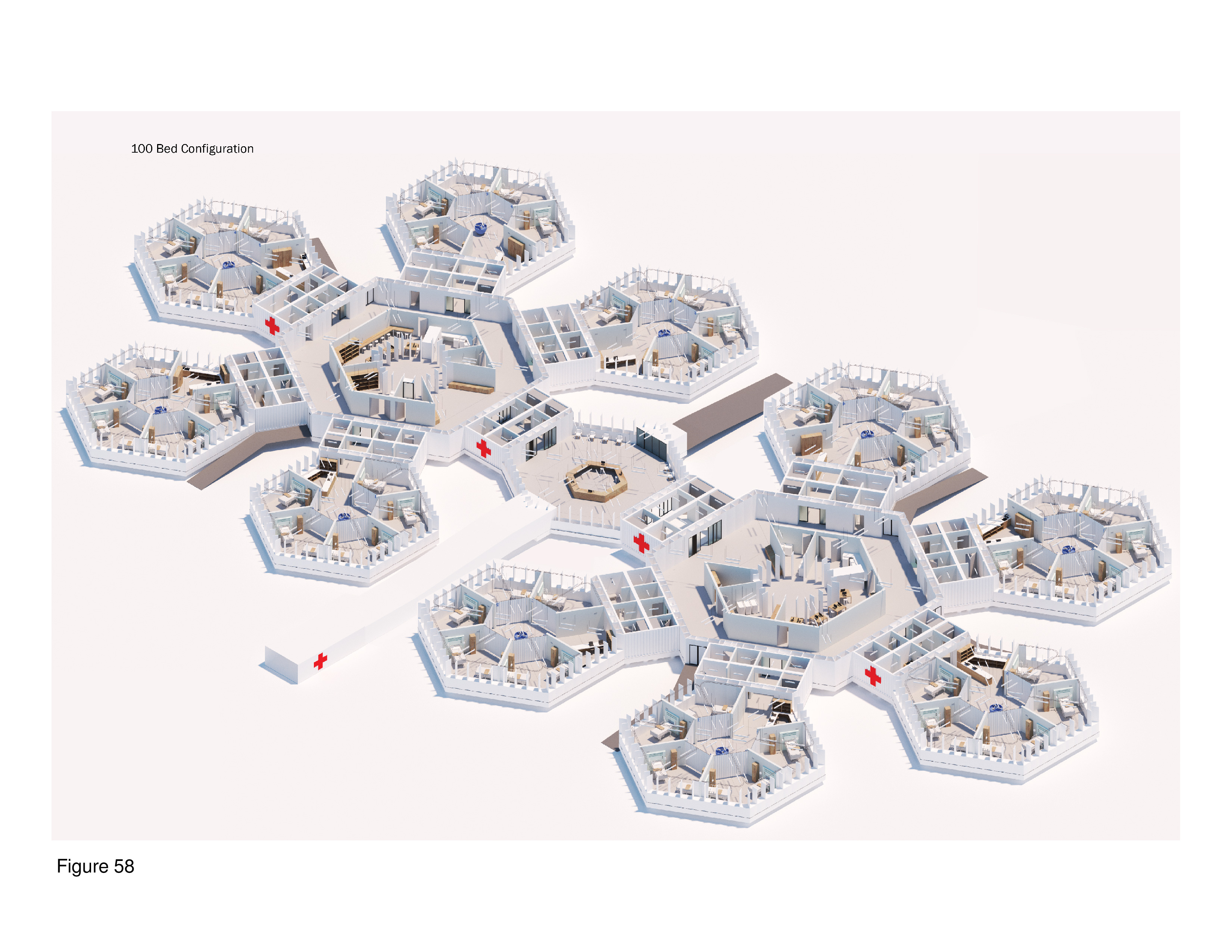
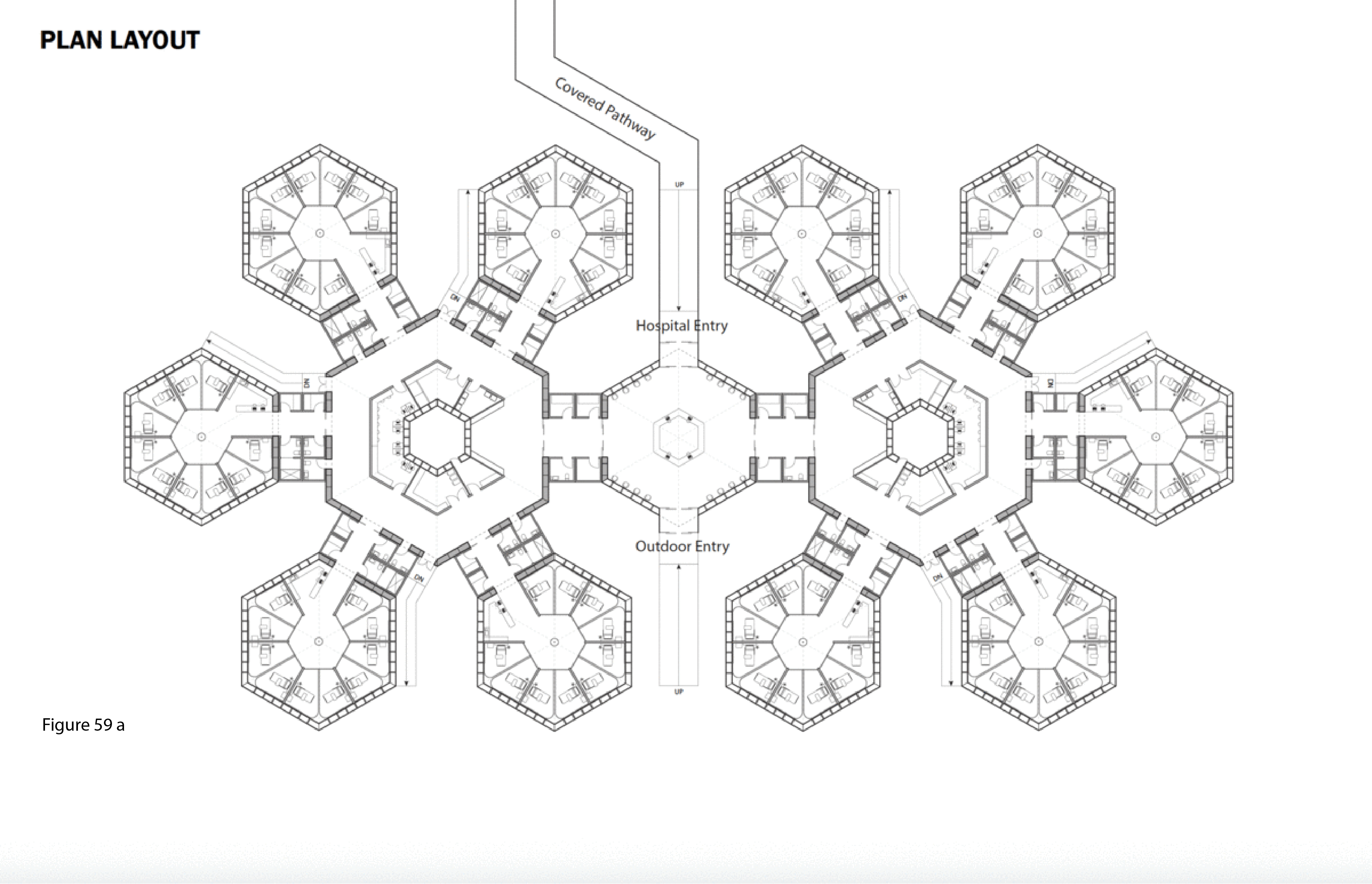
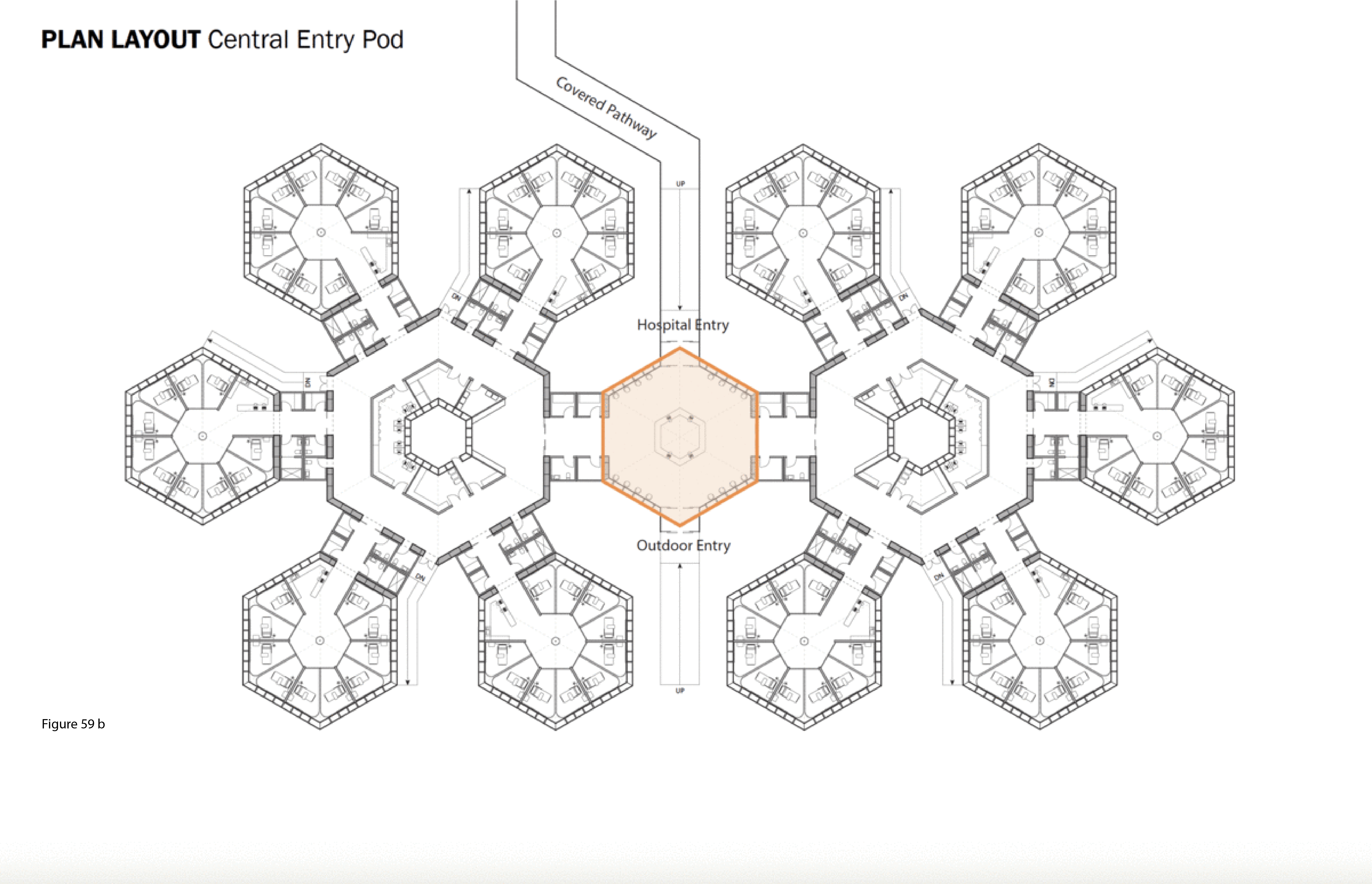
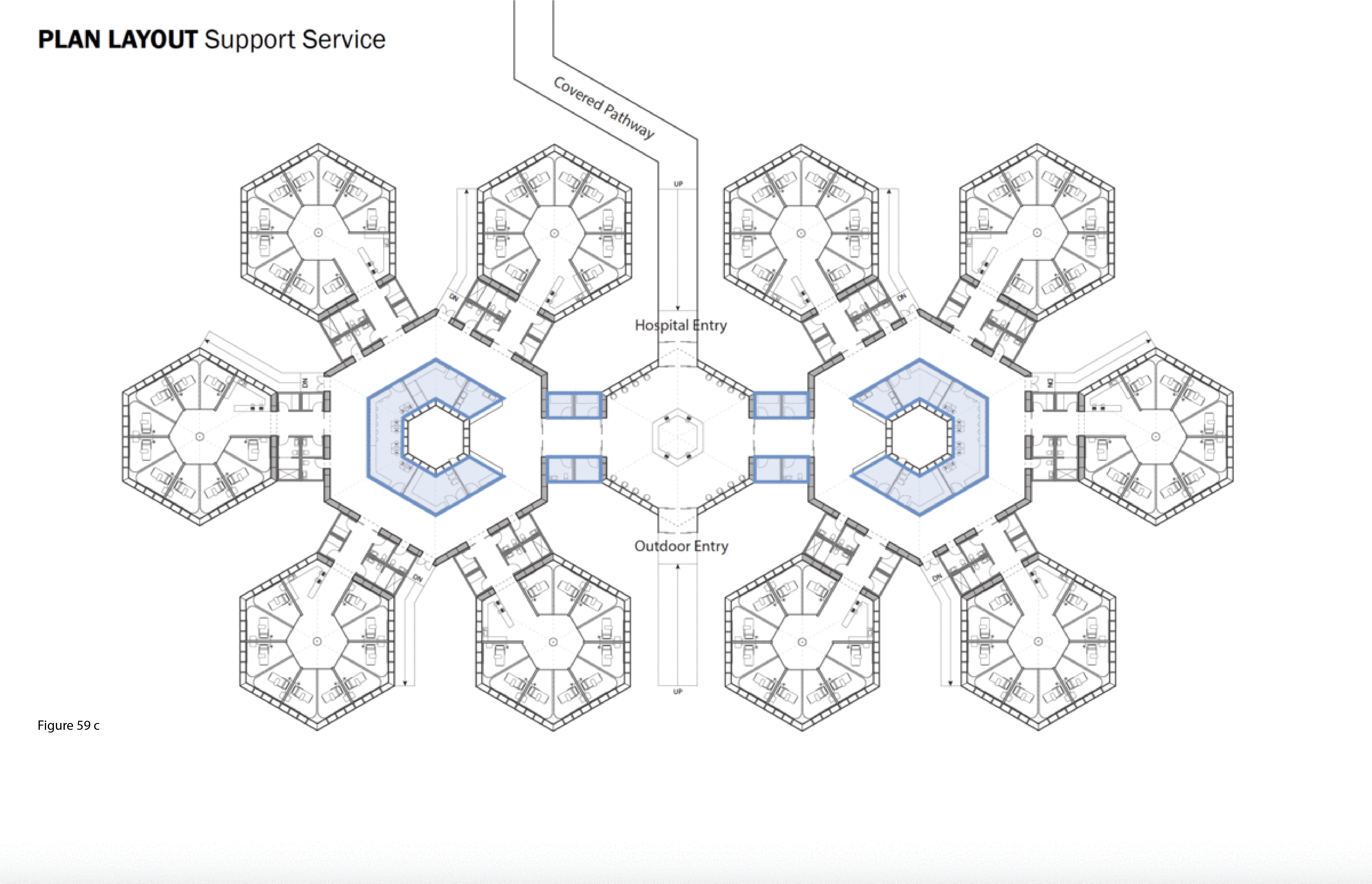
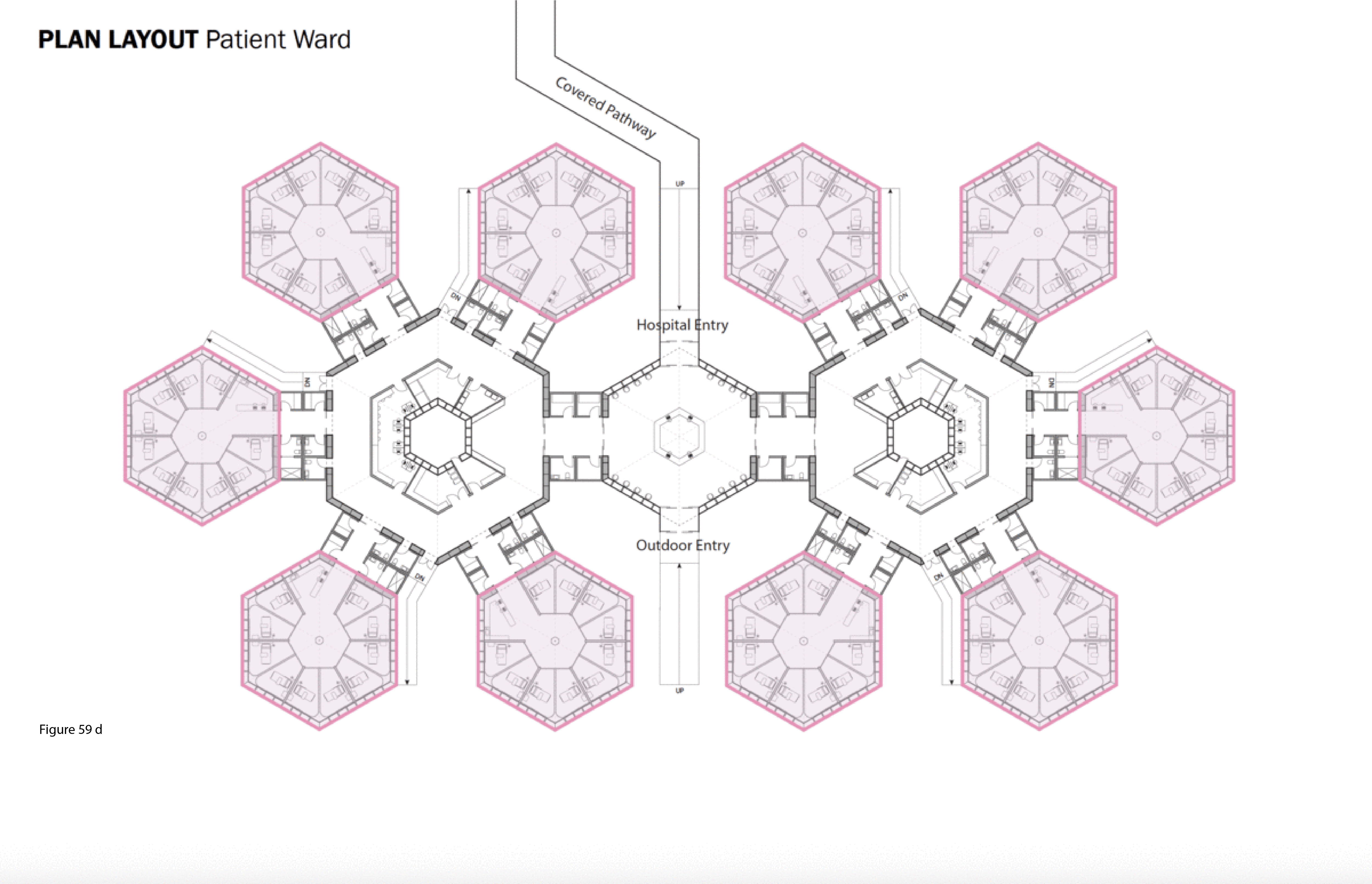
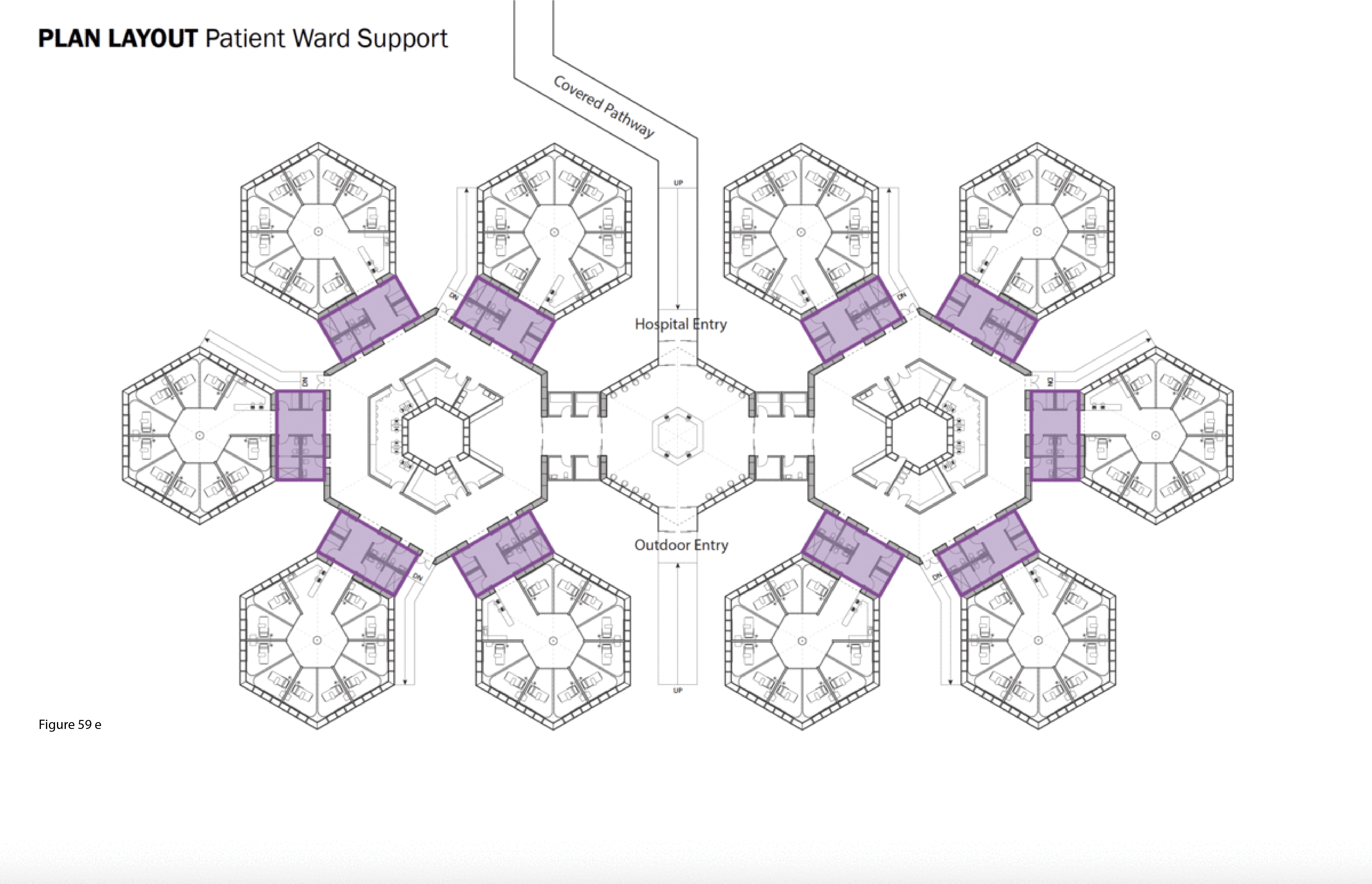
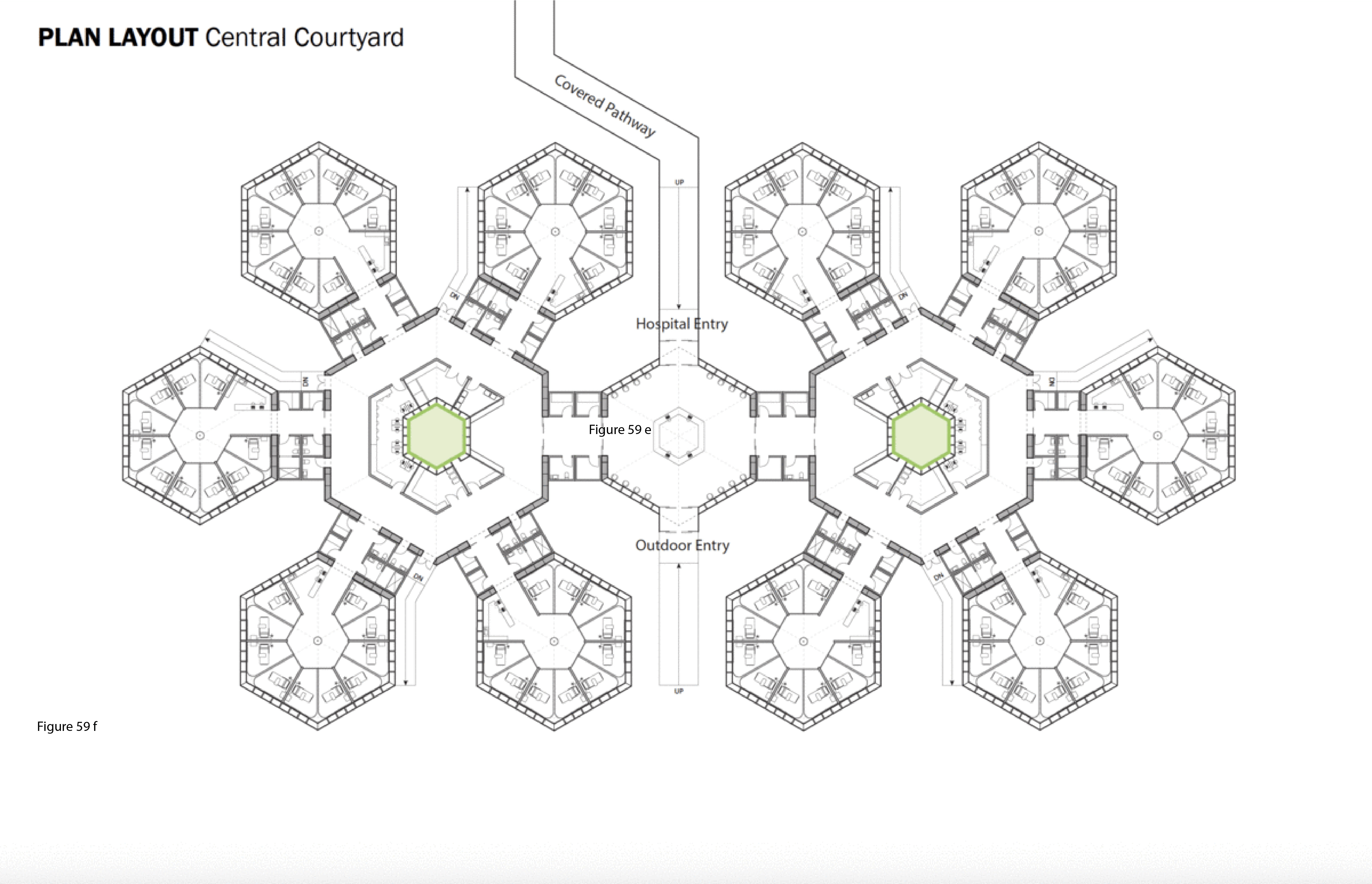
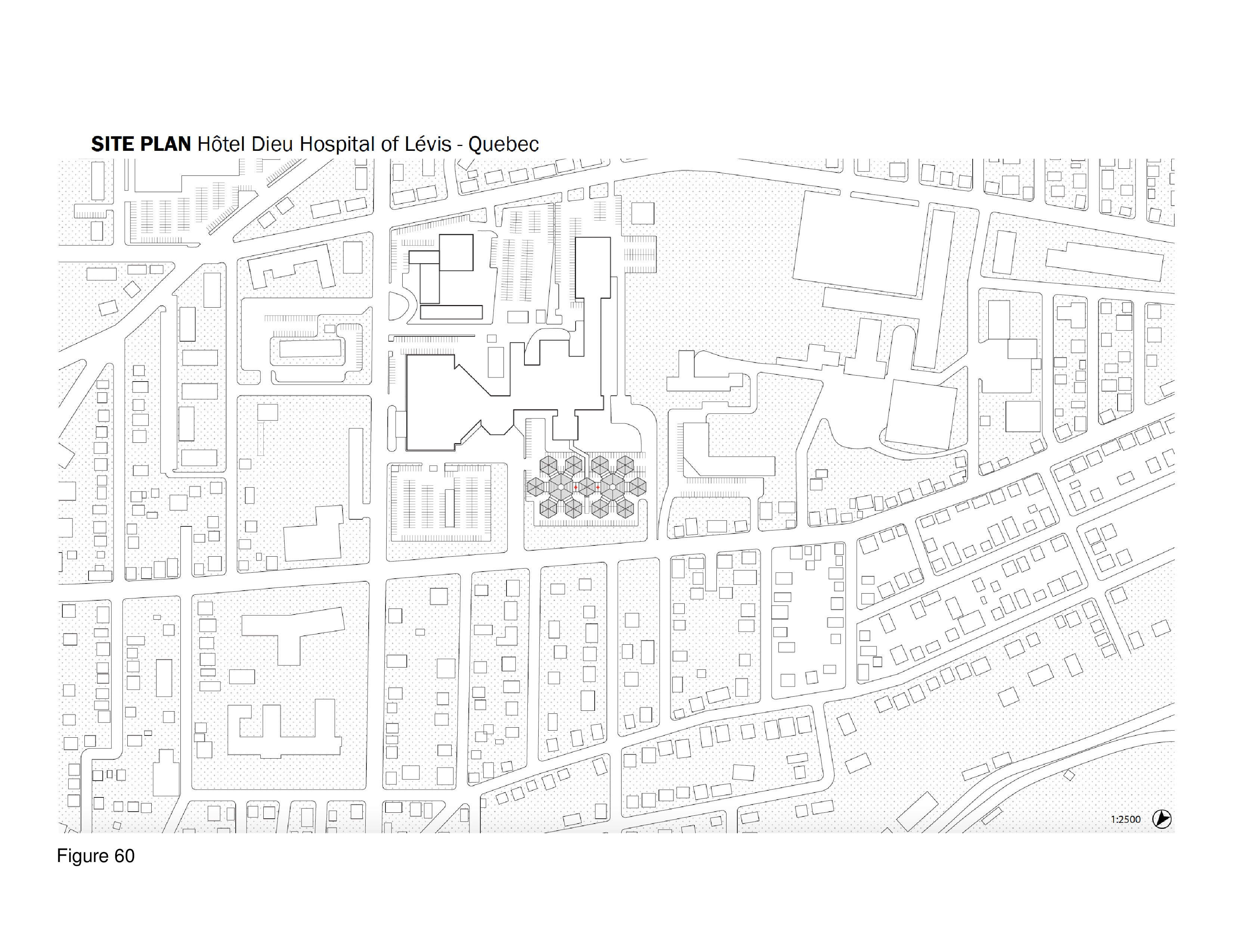
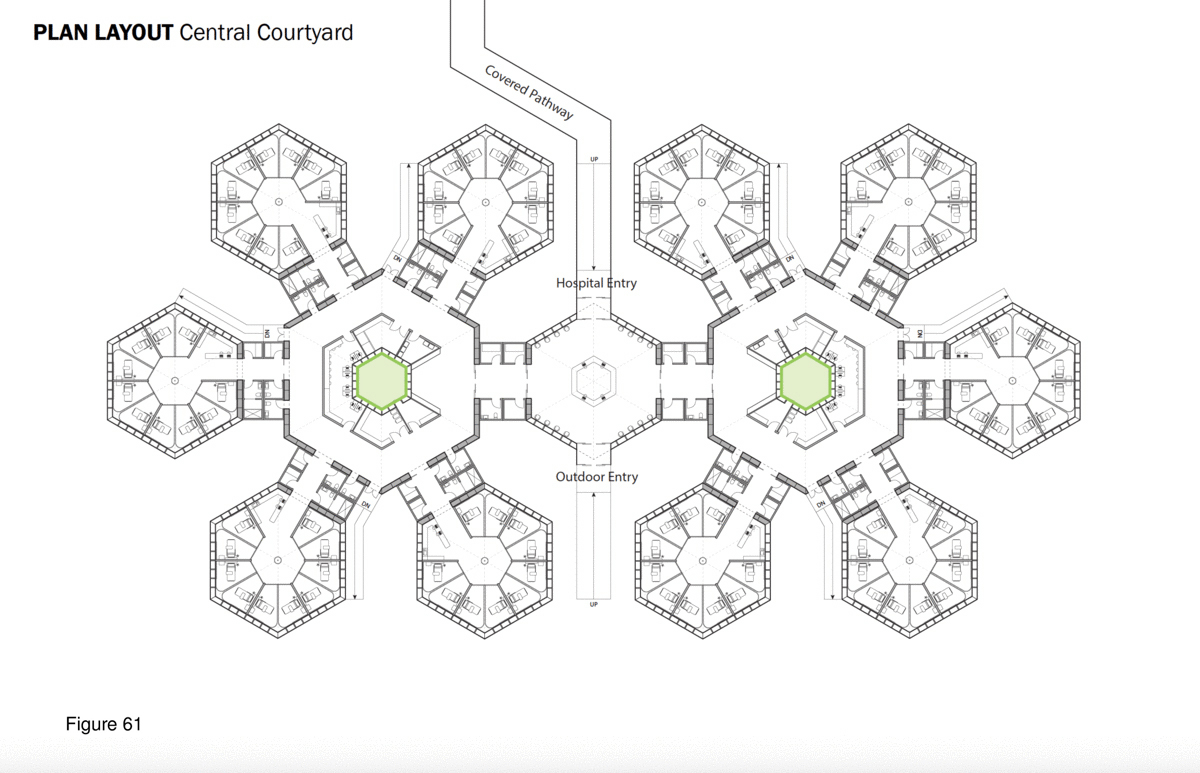
The SCH is a biophilia-inspired architectural response to arctic weather, transiting challenges routinely encountered in Canada’s circumpolar region, and deeply rooted vernacular building traditions in this region. This innovative system is flown in on cargo aircraft to the nearest airfield then trucked or airlifted via helicopter to the installation site. The architectural vocabulary is inspired by the indigenous building traditions of First Nations communities across Canada’s Far North. Low-to-the-earth, circular, healing lodges are traditionally known as sweat lodges. This healing precedent remains the preferred option in many Indigenous communities in Canada — as opposed to failure-prone, standardized, colonialist, i.e. Western, hospital building types and their associated medical practices.37 As for modernist precedents, Beloit General Hospital (Wisconsin, US), built in the late 1960s and designed by Flad Architects, is referenced here — it too was a snowflake, or snow crystal, in plan, presumably in reference to its snowy region. Beloit General was also a prominent example of American radiality during the 1960s in the U.S., along with Bertrand Goldberg’s now-demolished (2015) Prentiss Women’s Hospital (built 1974) at Northwestern University Medical Center in Chicago.38 A 100-bed configuration of the SCH is shown here installed at the Hôtel Dieu in Lévis, Quebec. Radial patient care healing houses contain 10 beds each, with privacy pull curtains separating beds not positioned along an outer wall, facing a central staff work core with hand sanitizing station and the nurse’s station. These modules plug into a custom-built shipping container housing staff and patient supports including washroom/shower, storage, mechanical/HVAC/IT, and staff restroom/shower. Aggregate “crystals” consisting of five radial pods each (10 by 5 feet) are in turn plugged into a common work zone which itself is plugged into the facility’s main arrival-intake module. This element houses central waiting/intake functions and receives the umbilical link from the acute care mothership. Every patient has a window that affords a view to the outside, and from the exterior, the forms and silhouette of the SCH is somewhat reminiscent of a First Nations village. (Figure 58, Figure 59a-f, Figure 60, Figure 61 and Figure 62a-b.)
COVID-19 Plug-in/Pop-out Hospital
Francesca Lu and Feibi Pan
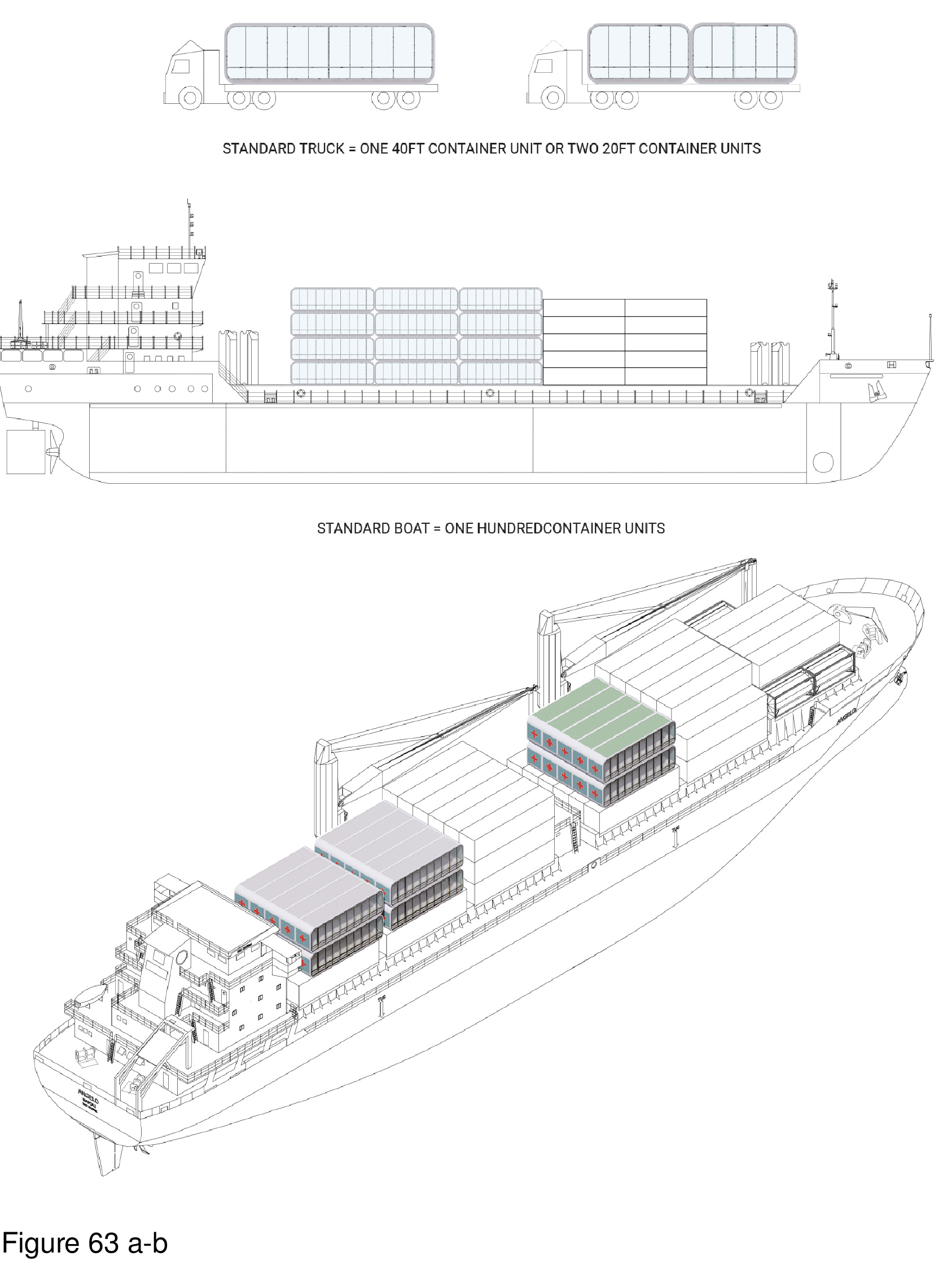
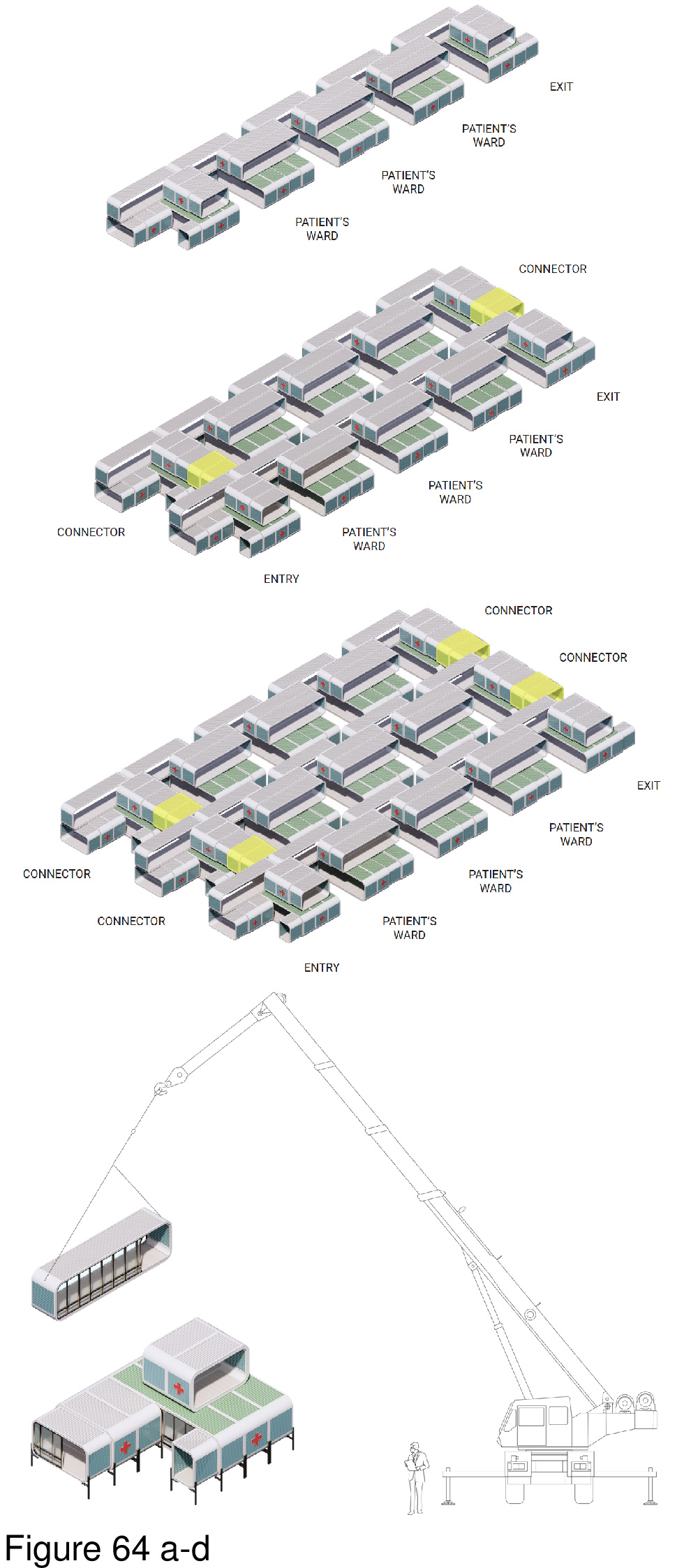
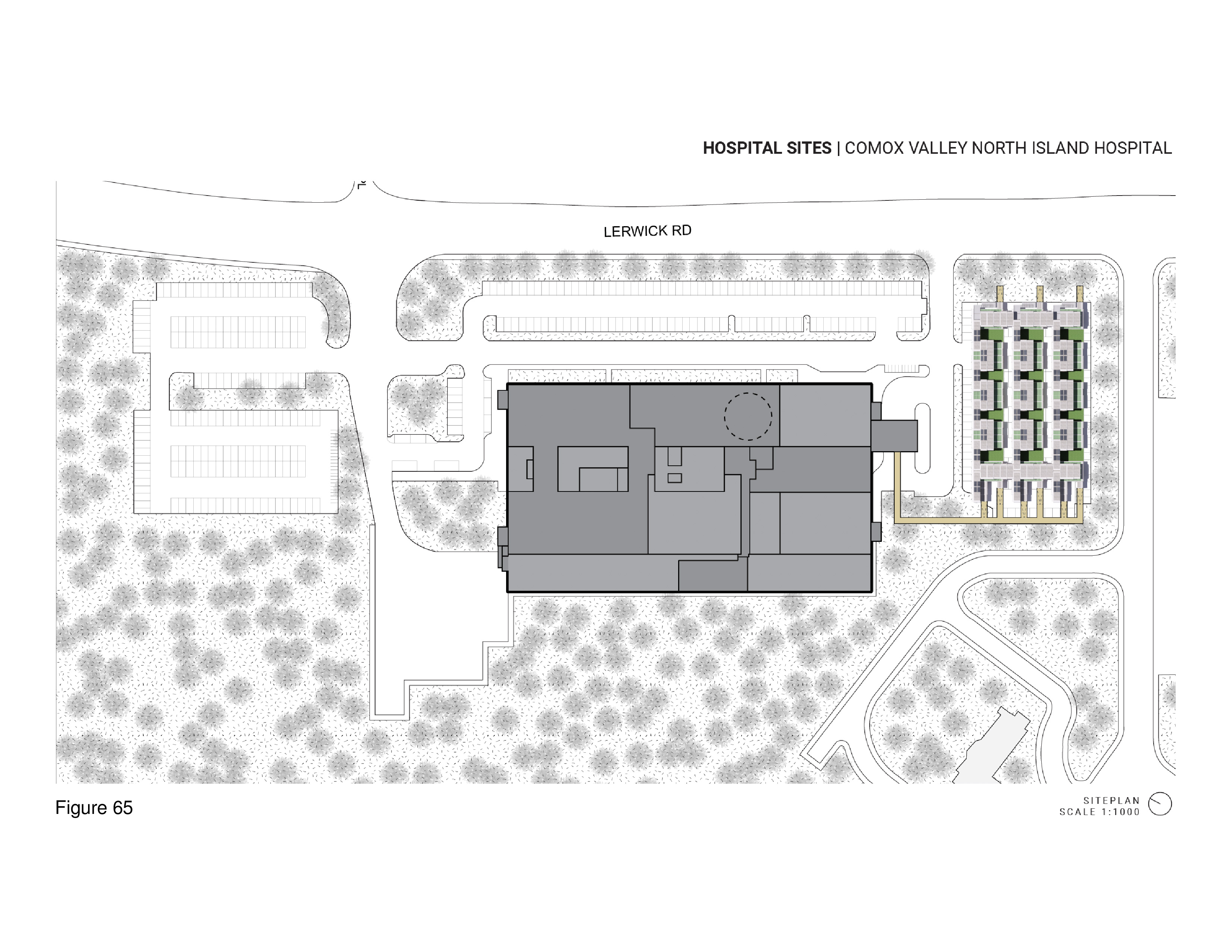
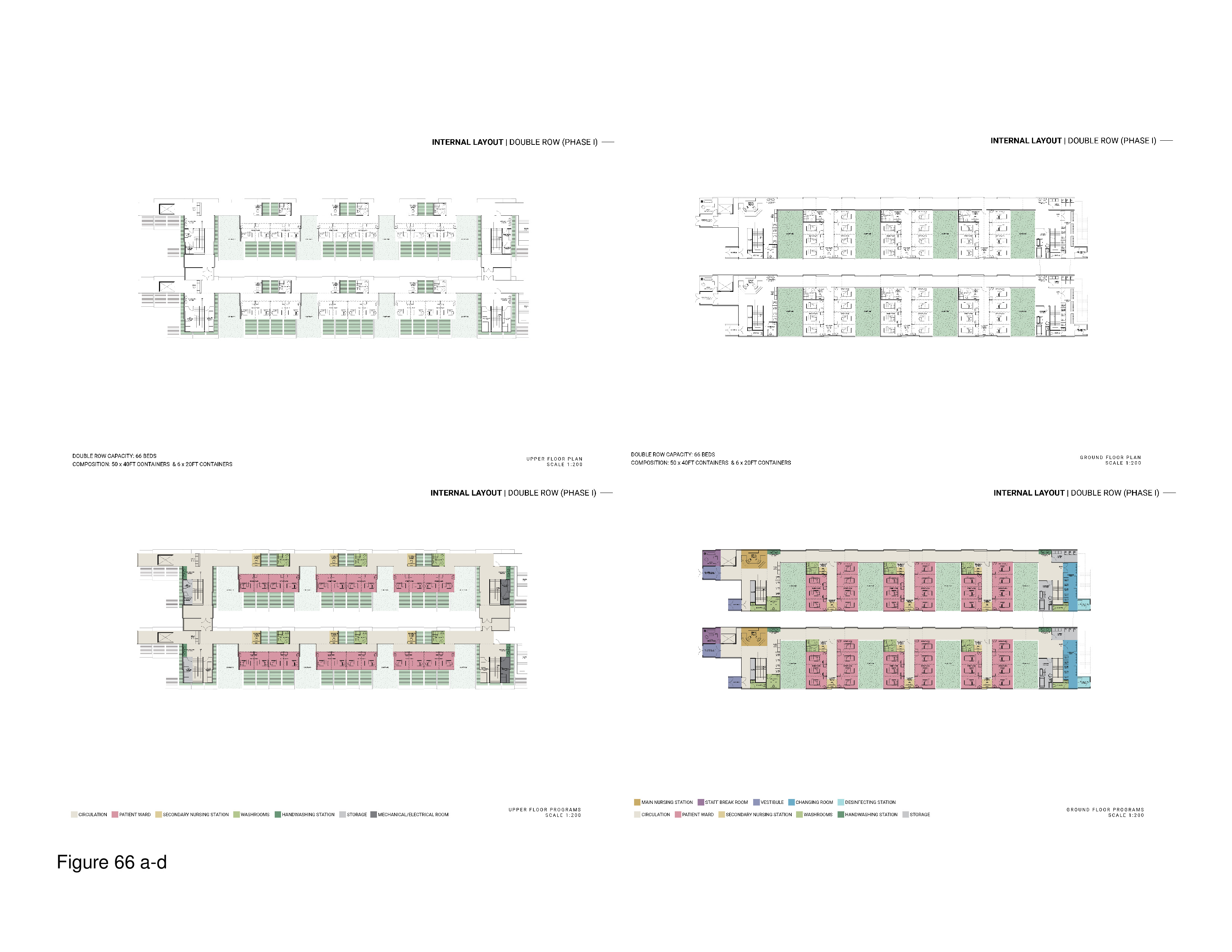
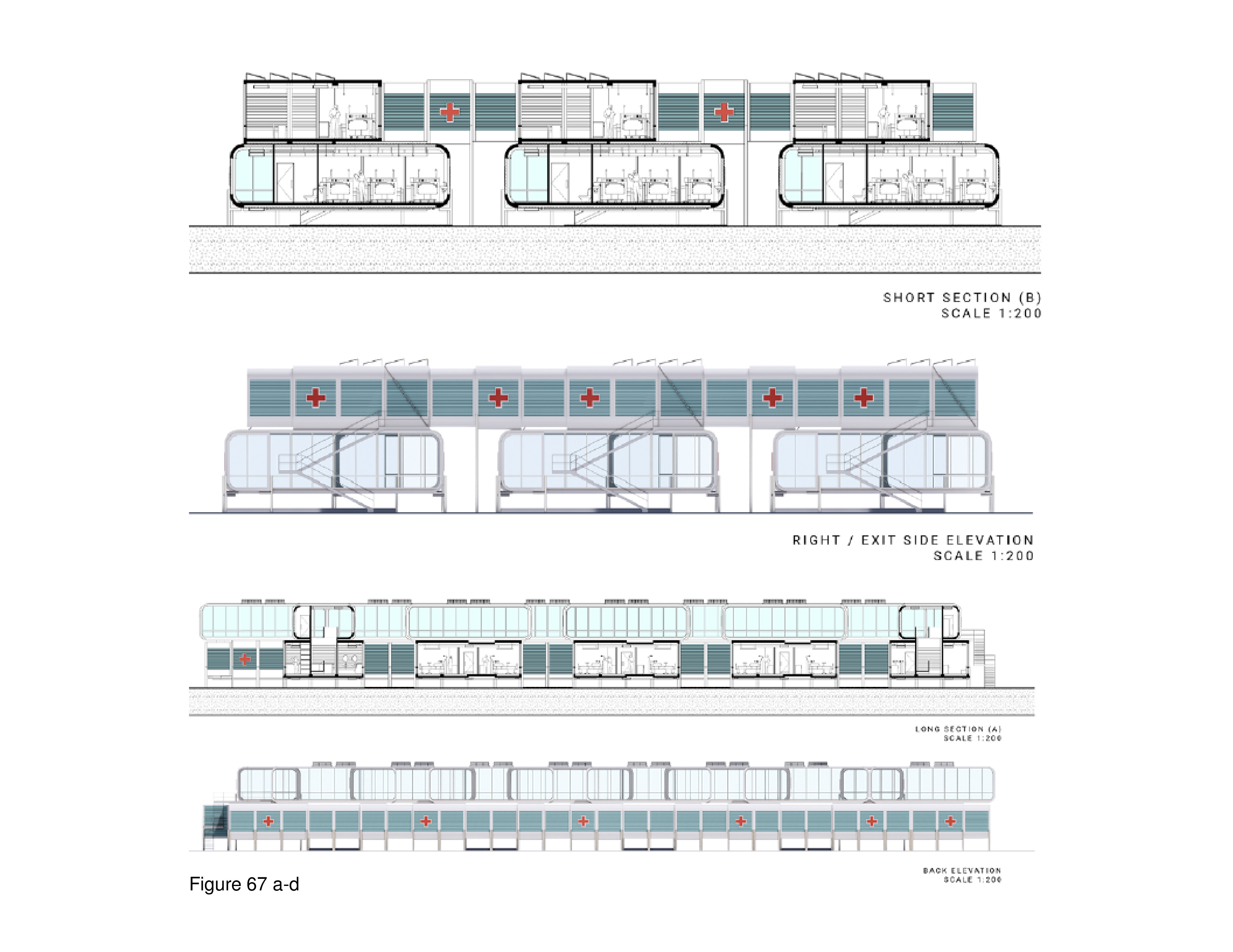
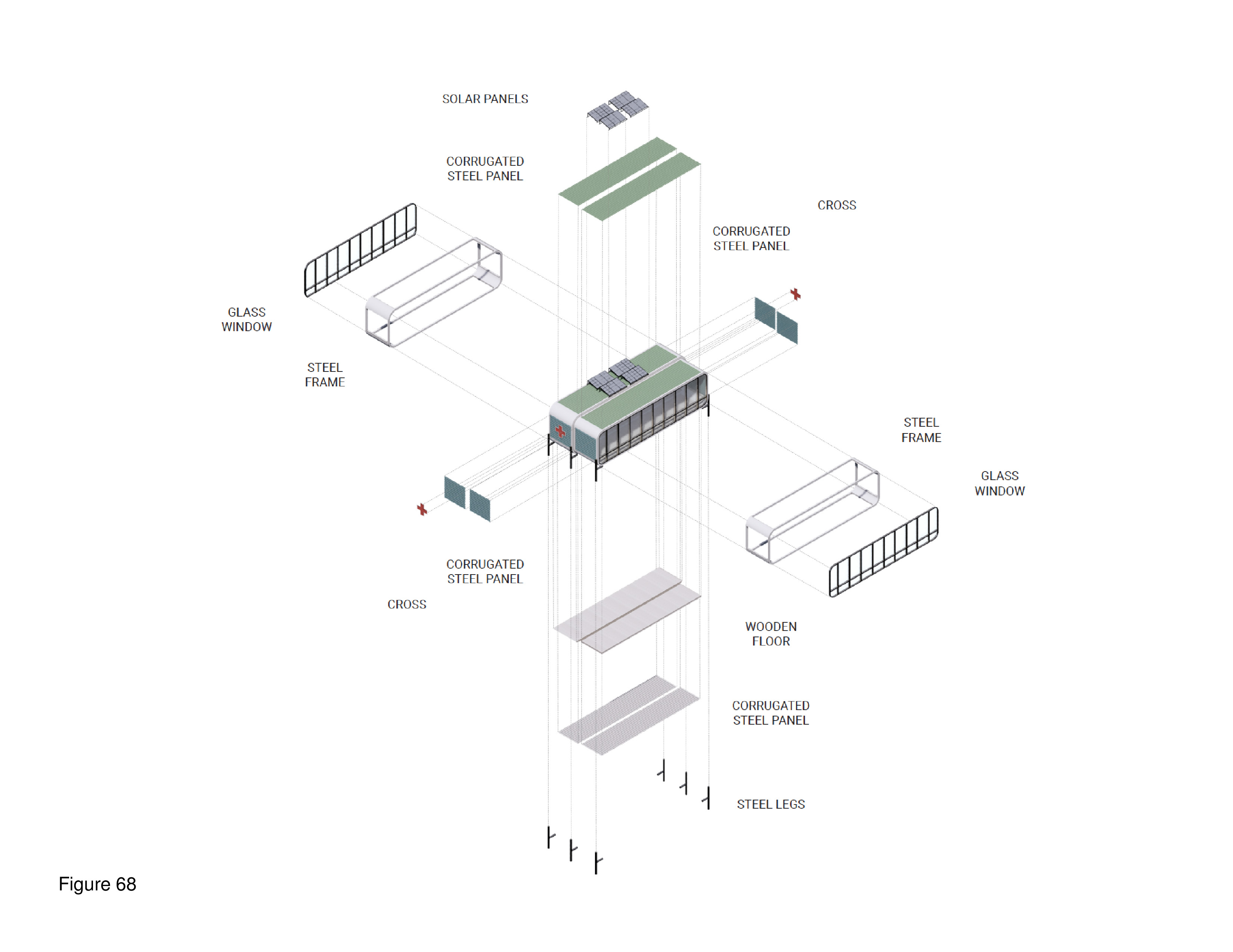
This portable, two-level system features interlocking containers with a pop-out element. In full deployment the containers form an A/B/A/B footprint punctuated by numerous mini-courtyards. In accord with biophilic tenets, and attention restoration theory, these exterior spaces allow occupants the opportunity to engage nature and landscape transmitting natural daylight to the interior. The containers are custom-built, transited in close-pack mode. They are locked together on site, iteratively, in either a 50-bed, 75-bed, or 100-bed configuration. The system shown here is proposed for installation on the campus of the Comox Valley North Island Hospital, in Courtenay, British Columbia. Solar panels are installed on site on the roof of the upper-level containers, where mechanical equipment is also housed. Patient beds are housed on both levels. An accompanying diagram illustrates this system’s kit of component parts, including those that are assembled to the container on-site. Transparency and spatial openness are of high priority, attributes incorporated as a reaction to the two entirely windowless COVID-19 ICU-surge hospitals built by the Chinese government in Wuhan, China in early 2020. Here, by contrast, many of the containers have full height windows; upper level containers overlook abstracted “green” (as in green painted) roofscapes of containers below — in reference to the actual green roofs that have become commonplace in non-portable medical facilities. HVAC, electrical, and plumbing systems run beneath the floor, and in ductwork suspended from ceilings. This plug/pop-out surge hospital is designed and manufactured for global deployment. (Figure 63a-b, Figure 64a-d, Figure 65, Figure 66a-d, Figure 67a-d, Figure 68, Figure 69a-b and Figure 70.)
A transportable is a prosthetic device
A transportable structure shares much in common with prosthetic devices worn by humans, such as artificial limbs. Both are built in a factory. Both are made of modular components and assembled in some sort of repetitive manufacturing process. Both must be lightweight, malleable, and adaptable to change in the face of sudden, and, at times, blunt force impact, and must be capable of returning resiliently to some approximation of their previous functional state prior to the disruption. Both must somehow continue to function should one module or wing (limb/system module) go down or offline temporarily. Both must be made (to the extent possible) of biodegradable parts in a way that minimizes ecologically harmful waste. Both must maintain fluidity so as to interdependently function while the larger system (human body/total installation) readjusts. Finally, both must remain operational and useful in diverse topographic and climatic conditions. Lightweight, advanced prosthetic devices are currently being researched in hundreds of research laboratories worldwide. If only the same could be said of their architectural corollaries.
Perhaps the COVID-19 pandemic has opened the door.
Any advancements will be predicated upon the ability of a transportable for health to fulfill a need in a given place while also being able to achieve the same elsewhere with the same system, if in a modified way. This is the fundamental design challenge.39
Three questions:
Is it feasible for transportable architecture to express the Vitruvian triumvirate of commodity, firmness, and delight?
Can this type of architecture provide more than minimal, baseline physical support in a major emergency?
What if transportable healthcare facilities were routinely designed and built to incorporate baseline as well as salutogenic and biophilic — that is, therapeutic — support in a time of crisis?
Salutogenic and biophilic affordances
Aaron Antonovsky, a medical sociologist, first defined the concept of salutogenics as the confluence of multiple positive factors supportive of human health and well-being. This flew in the face of then-prevailing, negativity-based definition of sicknesses and diseases traditionally associated with pathogenesis.40 The term salutogenesis is derived from the Latin salus, meaning “health,” and the Greek genesis, meaning “origin.” Antonovsky believed humans need and require cognitively supportive, meaningful environments in order to cope with highly stressful everyday situations — conditions that threaten to destroy our sense of place attachment in the world. He defined cognitive coherence as a three-faceted phenomenon consisting of comprehensibility, the belief that things occur in an orderly and relatively predictable manner allowing humans to reasonably predict future events; manageability, the belief that humans possess the capability to successfully solve problems and any given situation is therefore potentially soluble, and within one’s grasp and range of control; and life meaning, the belief that life, intrinsically interesting and a source of fascination, is worth living, with each person possessing a unique purpose and mission in life.41
The mental and physical challenge of being hospitalized for COVID-19 is intense. Jan A. Golembiewski and others have recently applied salutogenesis to the planning, design and daily management of psychiatric facilities. He argues that unsupportive, countertherapeutic, healthcare built environments challenge our physical and psychological coping abilities.42 In the context of COVID-19, comprehensibility is the principal lens through which the sick patient and one’s caregivers attempt to make sense of where one is, and why. Meaning is derived from the capacity to recognize and find interest in normalized elements from everyday life: a window with a view out, or a nature-scene mural. Attention restoration theory takes this further by recognizing that meaningful, positive distractions are needed while one is attempting to cope with a sudden, unfamiliar healthcare setting that is bad enough as it is. Isolation and disorientation can be mitigated, to a certain extent.
Biophilia is the human innate affinity, our natural predilection, for transactional relationships with nature. Its theoretical tenets have been explored in psychology and sociology since the 1980s in the work of Edward Wilson and others,43 including Stephen Kellert.44 In professional practice the therapeutic role of nature and landscape is being increasingly recognized by architects, landscape architects, and allied designers.45 This trend has accelerated in the thirteen years since publication of a literature review of evidence-based research in healthcare built environments.46 Kellert (2008) has defined the fundamental tenets of biophilic design as having two primary dimensions: organic or naturalistic, and place-based or vernacular. He defined six additional biophilic design elements: environmental features; natural shapes and forms; natural patterns and processes; light and space; place-based relationships; and evolved human-nature relationships.
In an oft-cited report, 14 Patterns of Biophilic Design, Browning, Ryan and Clancy (2014) outlined numerous biophilia-based design concepts that can help in promotion human health and well-being in the built environment:
Nature in space patterns (specifically, visual connectivity with nature, non-visual connections with nature, non-rhythmic sensory stimuli, thermal and airflow variability, the presence of water, dynamic and diffuse light, and connections with natural ecological systems).
Natural analogical patterns (specifically, biomorphic forms and imagery, materiality connections from or inspired by nature), and amelioration of discombobulation (overcomplexity versus patterned order).
Nature of the space patterns (specifically, prospect-refuge behaviours, the function of mystery and intrigue, and the role of risk-reward behaviors in relation to satisfaction and well-being).47
At this writing, no peer reviewed studies have been published examining the role of salutogenesis, or biophilic connectivity with nature during COVID-19 hospitalization. Evidence-based research is needed on these aspects of the staff and patient experience, as well as on best practices in patient and staff participation in the planning and design process, building tectonic innovations, and carbon neutral design, manufacture and construction strategies. Still, it is worthwhile to non-empirically review the twenty-four unbuilt and built projects discussed above through the translational lens of these design principles. Many of the walk-up/drive-up and 24/7 surge field hospitals reviewed appear, based on the evidence reviewed here, to suffer from these salutogenic and biophilic-related limitations:
- Lack patient confidentiality and privacy in waiting areas, and inadequate protective screening at pop-up testing stations.
- Lack of adequate circulation pathways that separate symptomatic from asymptomatic individuals awaiting testing or immunization, especially in pop-up facilities in repurposed host buildings.
- Inadequate staff workspaces and insufficient storage space for supplies such as PPE equipment, refrigerators, and laboratory equipment.
- Inadequate protection from the elements (weather) for persons availing themselves of outdoor testing and immunization pop-up facilities.
- Windowless conditions in 24/7 facilities precluding the occupant’s direct contact with natural daylight, views and ventilation, and inadequate artificial lighting options in support of attention restoration theory’s advocacy for positive multi-sensory distraction.
- An absence of representational or surrogate "nature views" and especially in insufficiently windowed spaces where a nature-themed mural, external window, window treatment, pull curtain, and/or actual plant could help to ameliorate a stressful physical setting.
- Monochromatic interior spaces difficult to navigate due to a confusing spatial layout, worsened by ineffective directional graphics.
- Overcrowded and under-designed patient housing zones, resulting in inadequate privacy and confidentiality, further compounded by a lack of bedside amenities
Granted, we are in the midst of a global health crisis. But if a higher level of pre-planning and design innovation had occurred, the present situation would not be as bad as it is.
Regardless, excuses abound:
“We didn’t have time to plan for anything like this.”
“We didn’t have the funds available on such short notice to consider windows, views, natural daylight or personal privacy.”
“My medical centre’s board of directors is unwilling to pay for an expensive portable infirmary that will probably just sit in some warehouse gathering dust for years.”
Architects are empowered by the clients and others who support and sponsor our thoughts and actions. Innovation cannot happen in a vacuum. A question for healthcare administrators and CEOs:
After this pandemic, will you just go back to the old ways of thinking when it comes to your healthcare facilities, or will you seriously consider the risk-reward benefits of portability as a compliment to old school brick and mortar facilities?
In point of fact, the University of Toronto graduate student projects endeavoured to incorporate salutogenic and biophilic qualities and features— experientially therapeutic — including visual connectivity with the exterior world vis-à-vis windows and views, plantings, nature-themed wall murals, transparency, symptomatic/asymptomatic patient circulation streams, clerestories, operable windows (where appropriate), color-coded entry-intake zones, layouts that foster wayfinding, umbilical connections with a mothership medical institution, and staff amenities such as break rooms. Spaces for family members were also provided in intake, waiting, and consultation. Are these “ideal” or optimal solutions? Of course, bugs would remain to be worked out in design development.
But at the very least, the best of the student and professional firms’ work reviewed above represents a viable, longer-term alternative to the knee-jerk, countertherapeutic repurposing of cavernous convention centres, sports arenas, and shopping mall parking lots.
Social responsibility and rapidity of response
In The Scope of Social Architecture, C. Richard Hatch (1984) viewed architectural education as an effective pedagogical vehicle for inculcating advocacy in serving the marginalized and the disenfranchised.48 He advocated that the professional must strive to fulfill unmet needs for equitable, affordable, dignified housing for underserved minority populations. He defined this as needing to think and act with rational transparency. Rational transparency is about addressing critical moral, ethical imperatives. Thomas Dutton, in citing the work of the educational theorists Roger Simon and Henry Giroux, reinforced Hatch’s advocacy position. He argued for inculcating a moral imperative where, in a world of needless pain and inequality, critical pedagogy in architectural education can and should value social justice, democracy, full equality, and social emancipation.49 This is attainable regardless of whether the curriculum is taken out to the problem (a health crisis, as in the case of COVID-19) or the problem is brought from the “real world” into the academy. Commitment and openness to advocacy through architecture to attain equitable health and social outcomes can be transformative.50
Le Corbusier recognized the architectural significance of the earliest transportable building type: the primitive temple was little more than a portable, nomadic structure consisting of crude poles covered in fabric or animal skins. It could be disassembled and relocated across deserts, grasslands and forests to the next place. To Le Corbusier, temporality embodied the essence of architecture: “There is no such thing as a primitive man, there are only primitive means.”51 Robert Kronenburg has cited the significance of ancient yurts as portable dwellings transited by mule or horse-drawn wagon. Seasonal factors weighed in, of course, as did the necessity of sudden relocation due to war, conflict, famine, and other adverse events:
“[There are] compelling arguments for moveable buildings…portable buildings, because of their dynamic nature [they] have the ability to play an active role in saving lives. Disaster relief is an obvious role…The lack of shelter in a post-disaster situation can lead to loss of life from exposure and disease that can be in excess of that caused by the disaster itself. It is essential that help [is forthcoming] in a very short time period, 48 hours or less, if that help is to be effective. Equally important…[are] facilities for medical [care]…deployable immediately to help nurture activities during reconstruction…based on an ecological…design strategy: buildings that ‘tread lightly on the earth’ and still convey that sense of identity and community so necessary in an established, responsible society.”52
Italo Calvino advocated for lightness as an essential tool of the designer in the 21st century.53 This is also what Shigeru Ban, winner of the 2014 Pritzker Prize in Architecture, has advocated. He pioneered the use of paper tubing as a structural design element in post-disaster housing and emergency shelters in projects throughout the world, including in the aftermath of the Tðhoku earthquake and tsunami in Japan (2011). In the heart of that strike zone he modified an overcrowded emergency shelter into an inhabitable space, with a relatively minor intervention. Importantly, his work personifies the ability to traverse back and forth across that line of demarcation separating non-elitist public interest architecture from commissions for well-heeled private clients. What does this mean for the education of future architects and for the profession itself?
A century ago, society experienced long periods of constancy and equilibrium punctuated by brief periods of radical change and upheaval — punctuated equilibrium. The current digital-right-NOW Information Age, in sharp contrast, is characterized by long spans of rapid, dramatic change punctuated by all-too-brief periods of relative constancy. This latter condition is referred to as punctuated chaos — periods of constant upheaval marked by brief respites.54
Politics, public health, medical science, and compassion are interwoven constructs.55 Whenever an architect whines about being under-respected it implies she or he may be disengaged from the most pressing matters of the day, somehow disconnected. And yet, indifference holds no reward in the face of a crisis like COVID-19. There is no silver bullet blueprint for achieving rational transparency and compassion in architecture. In uncertain times, practitioners, educators, social and mainstream media, and the general public jointly share responsibility. Granted, it is impossible to design a 100 per cent pandemic-proof architecture. This has been proven with respect to what happened in 24/7 residential long-term (nursing) care institutions for the aged across North America; death rates were disproportionally high in these facilities during the pandemic.
For the interested reader, an in-depth overview of the state of the art in transportable architecture for health is available in my recent book Innovations in Transportable Healthcare Architecture (2016). This book contains a brief history of transportable structures for healthcare from the 18th century to the present, a critical discussion of the challenges and rewards of prefab modularity, system transiting determinants, facility planning and design considerations that address the importance of salutogenic and biophilic design considerations, siting and building tectonic criteria, facility commissioning, and daily operations. The book concludes with a compendium of recent international unbuilt and built case studies.56 Fortunately, the University of Toronto Architecture+Health graduate design studio in fall 2020 was able to pivot in time to focus on prefabrication and lightness as key determinants in the context of the pandemic. Nonetheless, no claim has been made here that this review has been exhaustive. It could only serve as a broad brushstroke overview of how the international architectural community responded to a global public health crisis.
We architects need to do better
If one takes a look at the coronavirus pandemic’s impact in just one state in the U.S., Texas, the need for rapid response healthcare becomes evident. By January of 2021, state public health officials were warning that the pandemic was at its worst yet, with an average of more than 300 new deaths each day and a death toll of 33,176 since March of 2020. The state had administered most of its 1.7 million vaccine doses received to date, and was to receive 333,650 more doses. After businesses started to reopen the prior May, ICU hospitalizations increased dramatically. In response, the governor issued a statewide mandate requiring mask-wearing in public, but many completely disregarded this mandate. When the governor loosened restrictions on restaurants, bars and other businesses in cities and regions with steady hospitalization levels, the case count skyrocketed.

When cases in Texas increased further after the 2020 holiday season, public health experts and elected officials alike worried that loopholes had allowed bars and restaurants to prematurely reopen. That, combined with public fatigue contributed to the surge that was filling every Texas ICU bed in the state.57 More COVID-19 testing and immunization sites in shopping mall parking lots and sports facilities were called for.58 This was also the case at the repurposed Broadbent Arena in Louisville, Kentucky, home of Louisville’s icy hockey team. Its large doors and natural ventilation made it possible to quickly administer vaccine doses to hundreds of drive-up patients (Figure 71).59
Beginning with the first recorded pandemic, near modern-day Port Said in northeastern Egypt in 541, epidemiological crises have been by their very existence, disruptive. In their aftermath vast changes transformed societies affected. The Black Death of the 14th century (1340s) destroyed many aspects of everyday society.60 Of the roughly thirty universities that existed in Europe at that time, five were entirely wiped out. Only after the shockwaves subsided did the remaining universities in Europe gradually rebound.61 Interestingly, those emergencies fueled a shift away from a worldview centered on theology to one that increasingly valued science.
It is not a question of if another global pandemic or catastrophe will strike, but when. As David Wallace-Wells asserts in The Uninhabitable Earth: Life After Warming (2019), the compounded effects of coming catastrophes in this century will place unprecedented burdens on the planet’s healthcare infrastructure. By inference, he is referring to the need for advocacy-based public interest architecture, as part of the equation.62 For better or worse, our future is likely to be dominated more and more by the effects of pandemics, earthquakes, droughts, starvation, mass migration, hurricanes, typhoons and wildfires on steroids, the deleterious impacts of global sea level rise on coastal cities, and the depletion of non-renewable natural resources.63
In the 1960s, Martin Luther King Jr. frequently spoke of the need for thoughts and actions to be guided by radical empathy. This mindset requires fearlessness. It is about being unafraid to speak out and act upon what others don’t want to hear, ideas and actions others don’t really want to see happen because it is not in their personal best interest.64 Radical empathy has/had a place in architects’ response to the COVID-19 pandemic if for no other reason than it exposed longstanding health, racial, economic, and social inequities.65 Effective rapid response requires personal conviction, perseverance, and appreciation of timeless Vitruvian precepts calling for architecture as the provider of commodity, firmness, and delight in a civil, democractic society. The first two precepts alone are insufficient, if architecture is to be a meaningful participant. An advocacy-based architecture for health in the public, civic interest is worthwhile and achievable — especially in trying times.
Notes and references
1. Edelson, Zachery (2015) ‘Plague architecture: How designers have fought disease across the ages’, architizer.com. Available at https://architizer.com/blog/inspiration/collections/a-brief-history-of-… (accessed 12 October 2020).
2. Worldometers (2021) ‘COVID-19 coronavirus pandemic’, worldometers.info. Available at https://www.worldometers.info/coronavirus/?utm_campaign=homeAdvegas1.htm (accessed 25 January 2021).
3. Kurtz, Amir (2020) ‘An Israeli hospital set up an emergency care ward in 72 hours’, Calcalist. March 22. Available at https://www.calcalistech.com/ctech/articles/0,7340,L-3802859,00.html (accessed 11 November 2020). Also see Barcelona Convention Bureau (2020) ‘Vall d’Hebrón temporary hospital providing care for 132 COVID-19 patients’, Barcelona International Welcome. Available at https://www.barcelona.cat/internationalwelcome/en/noticia/first-tempora… (accessed 9 September 2020).
4. Otis, John (2020) ‘COVID-19 numbers are bad in Ecuador: The President says the real story is even worse’, National Public Radio. 20 April. Available at https://www.npr.org/sections/goatsandsoda/2020/04/20/838746457/covid-19… (accessed 10 May, 2020).
5. Fisher, Thomas (2008) ‘Public interest architecture: a needed and inevitable change’, In Bell, Bryan and Wakeford, Katie, Eds., Expanding Architecture: Design as Activism. New York: Metropolis Books: 1-4.
6. United Nations (2020) ‘Population’, United Nations. Available at https://www.un.org/en/sections/issues-depth/population/htm. (accessed 10 September 2020).
7. Fisher (2008): 2.
8. Ibid.: 3. Also see Frumkin, H., Frank, L., and Jackson, R. (2014) Urban Sprawl and Public Health: Designing, Planning, and Building for Healthy Communities. New York: Island Press.
9. Statista (2021) ‘Number of cumulative cases of coronavirus cases (COVID-19) worldwide from January 22, 2020 to January 19, 2021, by day,’ Statista.com. Available at http://www.statista.com/statistics/1103040/cummulative-covid19-cases-wo… (accessed 20 January 2021). By January, 2021, there were 96 million confirmed coronavirus cases worldwide, impacting more than 210 countries and territories with the United States accounting for nearly one-fifth of all confirmed cases. In the UK nearly 90,000, and in the United States more than 400,000 deaths had occurred. Health systems were overwhelmed. In the poorest countries millions lacked protective face masks, and hospitals lacked respirators. Clearly, additional intensive care unit (ICU) capacity was needed to care for the sickest as safe, effective testing sites to mitigate the pandemic as governments struggled with enforcement of lockdown restrictions.
10. M-RAD (2020) ‘COVID-19 mobile unit’, M-RAD. Available at https://www.m-rad.com/project/covid-19-mobile-unit/htm (accessed 12 October 2020).
11. Ravenscroft, Tom (2020) ‘Grimshaw designs range of shipping container coronavirus testing centres’, dezeen.com. 3 June. Available at https://www.dezeen.com/2020/06/03/grimshaw-shipping-container-coronavir… (accessed 1 October 2020).
12. MacLennan, Robin (2020) ‘Citizen Care Pods provide mobile COVID-19 testing and screening’, Ontario Construction News, 29 September. Available at https://www.ontarioconstructionnews.com/citizen-care-pods/htm (accessed 10 October 2020).
13. Perkins+Will (2020) ‘A COVID-19 mobile testing solution’, Perkins+Will. 21 April. Available at https://perkinswill.com/news/a-covid-19-mobile-testing-solution/ (accessed 1 October 2020).
14. Verderber, Stephen (2000) Healthcare Architecture in an Era of Radical Transformation. New Haven: Yale University Press: Chapter4.
15. plastique fantastique (2020) ‘Mobile PPS—Personal protective space for doctors. plastique fantastique. Available at https://plastique-fantastique.de/Mobile-PPS-for-Doctors (accessed 2 October 2020).
16. Opposite Office (2020) ‘Opposite office proposes to turn Berlin’s Brandenburg airport into COVID-19 Superhospital’, Opposite Office. Available at https://www.designboom.com/architecture/opposite-office-berlin-brandenb… (accessed 5 October 2020).
17. !INFEKT (2020) ‘CAMP-15: An eco-sustainable urban quarantine park’, !INFEKT. Available at http://www.infektural.com/EN/2020_02_CAMP15.html (accessed 2 October 2020).
18. Myers, Steven Lee (2021) ‘Facing new outbreaks, China places over 22 million on lockdown,’ The New York Times. 13 January. Available at https://www.nytimes.com/2021/01/13/world/asia/china-covid-lockdown.html (accessed 21 January 2021).
19. Ohly, Heather, White, Mathew P., Wheeler, Benedict W., Bethel, Alison, Ukoumunne, Obiola, Nikolaou, Vasilis and Garside, Ruth (2016) ‘Attention restoration theory: A systemic review of the attention restoration potential of exposure to natural environments’, Journal of Toxicology and Environmental Health, Part B, 19(7): 305-343. Available at https://www.doi.org/10.1080/10937404.2016.1196155 (accessed 15 January 2021).
20. Ottosson, J. and Grahn, P. (2005) ‘A comparison of leisure time spent in a garden with leisure time spent indoors: On measures of restoration in residents in geriatric care’, Landscape Research, 30(2): 23-55.
21. Wilson, Edward O. Biophilia. Cambridge, MA: Harvard University Press.
22. Kellert, Stephen R., Ed. (1993) The Biophilia Hypothesis. New York: Island Press.
23. Ulrich, Roger S., Zimring, Craig , Zhu, Xuemei, DuBose, Jennifer, Bo Seo, Hyun, Young, Seon Choi, Quan, Xiaobo, and Joseph, Anjali (2008) “A review of the research literature on evidence-based healthcare design’, Health Environments Research & Design Journal. 1(3): 61-125.
24. Kellert, Stephen (2008) ‘Dimensions, elements, and attributes of biophilic design’, In Kellert, Stephen and Heerwagen, Judith, Eds., Biophilic Design: The Theory, Science and Practice of Bringing Buildings to Life, Washington, D.C.: U.S. Green Buildooing Council. Also see Kellert, Stephen (2018) Nature by Design: The Practice of Biophilic Design. New Haven: Yale University Press.
25. Ryan, Catherine O., Browning, William D., Clancy, Joseph O., Andrews, Scott L., and Kallianpurkar, Namita B. (2014) ‘Biophilic design patterns: Emerging nature-based parameters for health and well-being in the built environment’, Archnet-International Journal of Architectural Research, 8(2): 62-76. https://earthwise.education/wp-content/uploads/2019/10/Biophilicdesign-… (accessed 25 June 2020).
26. Gillis, Kaitlyn, and Gatersleben, Birgatta (2015) ‘A review of psychological literature on the health and wellbeing benefits of biophilic design’, Buildings, 5(3): 948-963. Available at https://www.mdpi.com/2075-5309/5/3/948.htm (accessed 15 July 2020). Also see Verderber, Stephen and Peters, Terri (2019) ‘Integrating LEED with biophilic design affordances—Toward an inclusive rating system,” in Battisto, Dina and Wilhelm, Jacob J. Eds., Architecture and Health: Guiding Principles for Practice. London: Routledge, 2019: 311-327.
27. NCKU (2020) ‘NCKU, BAF co-design for COD-19 prototype of emergency quarantine hospital’, NCKU, 29 April. Available at https://web.ncku.edu.tw/p/406-1000-206984,r2845.php?Lang=en (accessed 4 October 2020).
28. futurarc (2020) ‘Modular design for mobile hospitals for the treatment of COVID-19’, futurarc.com. Available at https://www.futurarc.com/project/modular-design-of-mobile-hospitals-for… (accessed 3 October 2020).
29. Katsikopoulou, Myrto (2020) ‘AT-LARS completes prefab micro healthcare facility using scaffolding in Jakarta’, designboom.com. Available at https://www.designboom.com/architecture/at-lars-prefab-micro-healthcare… (accessed 3 October 2020).
30. Archdaily (2020) ‘Alternative healthcare facilities: Architects mobilize their creativity in fight against COVID-19’, archdaily.com. Available at https://www.archdaily.com/937840/alternative-healthcare-facilities-arch… (accessed 4 October 2020).
31. Griffiths, James, Sidhu, Sandi and Gan, Nectar (2021) ‘WHO team in Wuhan to begin long-delayed coronavirus investigation after clearing quarantine’, CNN. January 26. Available at https://www.cnn.com/2021/01/26/asia/who-coronovirus-team-wuhan-china/htm (accessed 26 January 2021).
32. Wang, Jessica, Zhu, Ellie, and Umlaut, Taylor (2020) ‘How China built two coronavirus hospitals in just over a week’, Wall Street Journal, 6 February. Available at https://www.wsj.com/articles/how-china-can-build-a-coronavirus-hospital… (accessed 15 February 2020).
33. HaHa Architects Group (2020) ‘Field rescue center’, HaHa Architects Group. Available at http://hahagroup.pl/Field-Rescue-Center.php (accessed 4 October 2020).
34. Ravenscroft, Tom (2020) ‘Shipping container intensive care unit installed at Turin hospital’, dezeen. 21 April. Available at https://www.dezeen.com/2020/04/21/shipping-container-intensive-care-uni… (accessed 12 October 2020).
35. HGA (2020) ‘STAAT MOD critical care units address COVID-19 hospital bed shortage’, HGA. Available at https://hga.com/staat-mod-critical-care-units-address-covid-19-hospital… (accessed 3 October 2020).
36. Archdaily (2020) ‘Monash Health RESUS Facility/SPACECUBE’, archdaily.com. Available at https://www.archdaily.com/943908/monash-health-resus-facility-spacecube… (accessed 4 October 2020).
37. Verderber, Stephen, Skouris, Eric, and Wolf, Jacob Pauls (2020) ‘Indigenous ecohumanist architecture for health in Canada’s Far North’, Health Environments Research & Design Journal, 13(4): 210-224.
38. Verderber, Stephen and Fine, David J. (2000) Healthcare Architecture in an Era of Radical Transformation: Chapters 2-4.
39. Verderber, Stephen (2016) Innovations in Transportable Healthcare Architecture. London and New York: Routledge. Also see Guenther, Robin and Vittori, Gail (2013) Sustainable Healthcare Architecture. Second Edition. New York: John Wiley.
40. Antonovsky, Anton (1979) Health, Stress and Coping. San Francisco: Jossey-Bass Publishers.
41. Verderber, Stephen (2018) Innovations in Behavioural Health Architecture. London: Routledge: 108.
42. Golembiewski, Jan A. (2012) ‘Psychiatric design: Using a salutogenic model for the development and management of mental health facilities’, World Health Design, 5(2): 74-79.
43. Wilson, Edward O. (1984) Biophilia. Cambridge, MA and London,UK: Harvard University Press.
44. Kellert, Stephen (1997) The Value of Life. Washington: Island Press.
45. Gillis and Gatersleben (2015).
46. Ulrich, et al. (2008).
47. Browning, W.D, Ryan, C.O., and Clancy, J.O. (2014) ’14 Patterns of Biophilic Design’, New York: Terrapin Bright Green, LLC. Also se Barton, Sophie (2019) ‘Biophilic design: Bill Browning explains the dramatic impact it has on wellbeing’, workinmind.com. Available at https://workinmind.org/2019/02/20/biophilic-design-bill-browning-explai… (accessed 12 January 2021).
48. Hatch, C. Richard (1984) The Scope of Social Architecture. New York: Van Nostrand Reinhold.
49. Dutton, Thomas (1996) ‘Cultural studies and critical pedagogy,’ In Dutton, Thomas and Mann, Lian Hurst, Eds. Reconstructing Architecture: Critical Discourses and Social Practices. Minneapolis: University of Minnesota Press: 158-201. Also see Sholle, David (1992) ‘Authority on the left: Critical pedagogy, postmodernism and architecture’, Cultural Studies, 6(2): 272-273.
50. Verderber, Stephen (2003) ‘Compassionism in the design studio in the aftermath of 9/11’, Journal of Architectural Education, 52(3): 48-62.
51. Le Corbusier (1984 Translation) Toward a New Architecture. Etchells, Frederick, Translator. New York: Holt, Rinehart and Winston.
52. Kronenburg, Robert (1995) Houses in Motion: The Genesis, History and Development of the Portable Building. London: Academy Editions.
53. Calvino, Italo (1988) ‘Lightness’, In Six Memos for the Next Millennium. Cambridge: Harvard University Press: 3.
54. Gates, Bill with Hemingway, Collins (1999) Business @ the Speed of Thought. New York: Warner Books: 411-412.
55. Verderber (2003): 58.
56. Verderber (2016): Chapters 4 and 5.
57. Brooks-Harper and Najmabadi, Shannon (2021) ‘Texas has a problem with its COVID-19 vaccination data, and the stakes are high. How the state is scrambling to solve it’, Texas Tribune, 20 January. Available at http://www.texastribume.org/2021/01/20texas-coronovirus-vaccine-date/htm (accessed 21 January 2021).
58. Brooks-Harper, Karen and Canizales, Anna (2021) ‘Progress in the fight against the coronavirus is coming, but Texas is a long way from herd immunity’, Texas Tribune, 1 February. Available at https://www.texastribune.org/2021/02/01texas-coronavirus-herd-immunity/… (accessed 1 February 2021).
59. Wright, Will and Cherry, Jon (2021) Forty hours later, a shot at a vaccine’, The New York Times, 3 February. Available at https://www.nytimes.com/interactive/2021/02/03/multimedia/virus-vaccine… (accessed 4 February 2021).
60. Dennis, Marguerite (2020) ‘Higher education opportunities after COVID-19’, University World News. 9 May. Available at https://www.universityworldnews.com/post.php?story=20200507152524762.htm (accessed 20 January 2021).
61. Witza, Alexandria (2020) ’Universities will never be the same after the coronavirus crisis’, Nature.com. 1 June. Available at https://www.nature.com/articles/d41586-020-01518-y.htm (accessed 22 January 2021).
62. Wallace-Wells, David (2019) The Uninhabitable Earth: Life After Warming. New York: Tim Duggan Books.
63. Hancock, Trevor (2016) ‘Healthcare in the Anthropocene: Challenges and Opportunities’, Healthcare Quarterly, 19(3): 17-22.
64. Lu, Denise and Flavelle, Christopher (2019) ‘Rising seas will erase more cities by 2050, new research shows’, The New York Times, 29 October. https://www.nytimes.com/interactive/2019/10/29/climate/coastal-cities-u… (accessed 3 January 2020).
65. Stiglitz, Joseph (2020) ‘Conquering the great divide’, International Monetary Fund. Finance & Development Report, Fall. Available at https://www.imf.org/external/pubs/ft/fandd/2020/09/COVID19-and-global-i… (accessed 25 January 2021).
Acknowledgements
Thanks to all the firms who granted permission to reproduce their drawings and photo images. Thanks also to my research assistants, Damian Kercz and Shivathmikha Suresh Kumar, for their help during the literature review and in identifying firms’ architectural projects internationally. Thanks to the students in the Fall 2020 Architecture + Health Graduate Design Option Studio (ARC 3020YF L9101) at the University of Toronto, for their commitment to the urgent nature of the task at hand. Research funding was provided by the University of Toronto Daniels Faculty of Architecture, Landscape, and Design. Figure 71 courtesy the New York Times.
Citation: Verderber, Stephen (2021) Pandemical Healthcare Architecture and Social Responsibility--COVID-19 and Beyond. Centre for Design+Health Innovation White Paper, 26 February 2021. University of Toronto. https://www.daniels.utoronto.ca/pandemical-healthcare-architecture-and-…
Copyright, 2021, Stephen Verderber and the University of Toronto.