Reimagining Long-Term Care Architecture in Post-Pandemic Ontario—and Beyond (Part II)
Introduction
Long-term care (LTC) residential built environments are complex with no single definition that aptly captures their typological variability. They operate in diverse geographic, socio-cultural, and political contexts and are regulated by multiple governmental agencies with licensure oversight for health and human welfare minimum compliance. Daily operations are further subject to oversight by third-party accreditation commissions. There is no single set of architecturally-related issues considered to be ‘universal.’ However, certain time-tested patterns are discernable across time and space, patterns rooted in salutogenic and biophilic design concepts regarding the planning, design, construction and daily operation of LTC homes: Fifty design considerations are presented, for broad interpretation by architects, landscape architects, interior designers, planners, engineers, sustainability and resiliency specialists, direct caregivers including physicians, psychiatrists, allied therapists, gerontologists, nurses and allied support staff, administrators, Boards of Directors, federal and provincial government agencies, private philanthropic foundations, grassroots eldercare advocacy organizations, elected officials, health policy specialists and public health agencies.
These design considerations are inspired by the work of Christopher Alexander and the classic A Pattern Language: Towns, Buildings, Construction (London: Oxford University press, 1977, and subsequent editions). The genius of this method is that an individual pattern is nested within other patterns, here connected by hyperlinks forming a relational web-network. This approach was the inspiration for Wikipedia and other software algorithms including Agile, Extreme Programming, and Scrum. As with the first Pattern Language (1977) each design consideration is accompanied by one or more research citations drawn from the environment and aging literature published since January of 2005. After each, other pertinent design considerations are cited with a link. Note: These literature sources are listed thematically in Part III (below) with the exception of the references highlighted with an asterisk * Also, a reference identified bold is accompanied with a link to its PDF. References are listed in alphabetical order following each design consideration.
This compendium is inspired by the Ontario Long-Term Care Home Bill of Rights and its 27 core provisos:
“1. Respect and dignity; 2. No abuse: 3. No neglect; 4. Proper care; 5. Safe and clean home: “You have the right to have a safe and clean place to live in;” 6. Citizen’ rights; 7. Knowing your caregivers; 8. Privacy: “You have the right to privacy;” 9. Participation in decisions; 10. Personal belongings: “You have the right to keep personal things in your room. This is your home. As in any home, it is important to have personal items around that are special to you or make you feel more comfortable;” 11a. Plan of care; 11b. Consent to treatment; 11c. Care decisions; 11d. Privacy and health information; 12. Independence: “You have the right to get help to become as independent as you can. For example, you have the right to get help to improve your ability to walk or go to the bathroom on your own;” 13. Restraint; 14. Communicate and visit in private; 15. Visitors during critical illness; 16. Designated contact person; 17. Raising concerns; 18. Friendships: “You have the right to make friends and to spend time with them. You have the right to be involved in any activities offered at the long-term care home, if you wish;” 19. Lifestyle and choices: “You have the right to live your life in the manner you wish;” 20. Residents’ council; 21. Intimacy: “You have the right to be alone with your spouse or a person who is important to you;” 22. Sharing a room: “You have the right to share a room with another resident, so long as you both agree and space is available at the home;”23. Personal interests; “You have the right to do things that interest you and things that are important to you, either inside or outside the home;” 24. Written policies; 25. Your money; 26. Going outside: “You have the right to go outside to enjoy nature, fresh air, and outdoor activities whenever possible. If the home has a protected area, no one can stop you from using it;” and 27. Bringing people to meetings. What can I do if my rights are violated? Getting legal help and information.” FN Community Legal Education Ontario (2022). Bill of Rights for People Who Live in Ontario Long-Term Care Homes. CLEO. https://www.cleo.on.ca/en/publications/everyres.
The aim is for others to build upon this compendium to improve the architectural and landscape design quality of LTC environments for the aged. More evidence-based research is needed. Evidence-based environment and aging knowledge and designing for aging are inextricably interwoven. It is hoped the reader will view each design consideration as a hypothesis. The nine themes are: Site Context and Spatial Organization (1), The Private Realm (2), The Shared Realm (3), Biophilia and Nature Connectivity (4), Circulation and Navigation (5), Support Amenities (6), Sensory and Environmental Support (7), Offsite Prefabrication (8), and Total Support (9):
Table of Contents
1. SITE CONTEXT + SPATIAL ORGANIZATION
1a. Proximity to Infrastructure
1b. Maximize Parti’ Logic
1c. Mixed-Use Campus
1d. Elderesidence Imagery
1e. Hierarchical Realms
1f. Decentralized Houses
2. PRIVATE REALM
2a. Medically Safe Bedrooms
2b. Balconies and Patios
2c. Personalization and Distancing
2d. Universal Washrooms
3. SHARED REALM
3a. Kitchen and Dining Areas
3b. Prospect-Refuge Imperatives
3c. Foster Everyday Activities
3d. Functional Adaptation
4. BIOPHILIA—NATURE CONNECTIVITY
4a. Age Appropriateness
4b. Roof Terraces
4c. Horticultural Therapy
4d. Multiple Outdoor Destinations
4e. Ecological Stewardship
4f. Natural and Mechanical Ventilation
4g. Theraserialization
4h. Habitat Conservation
5. CIRCULATION + NAVIGATION
5a. Wayfinding and Orientation
5b. Controlled Wandering
5c. Programmatic Decompression
5d. Single Loaded Circulation—Residential Zones
5e. Universal Accessibility
6. SUPPORT AMENITIES
6a. Maximize Caregiver/Family Supports
6b. Artificial Intelligence
6c. Intergenerational Connections
6d. Aging in Place in the Far North
7. SENSORY + ENVIRONMENTAL SUPPORT
7a. Differentiated Surfaces and Materiality
7b. Eliminate Institutional Cues
7c. Dynamic and Diffuse Light/Lighting
7d. Noise Abatement
7e. Ambient Environment—Comfort
7f. Multisensory Stimulation
8. OFFSITE PREFABRICATION
8a. Destigmatizing Modular Prefabrication
8b. Building in the Far North
8c. Accessory Dwelling Units
9. TOTAL ENVIRONMENT
9a. Site Selection and Health Promotion
9b. Engage the Local Community
9c. Resident and Caregiver Safety
9d. Constituency Empowerment
9e. Net-Zero Strategies
9f. Evidence-based Research for Design
9g. Disaster Preparedness and Resiliency
9h. Ecohumanism and Cost Containment
9i. Preparatory Design Strategies—Covid-19 and Beyond
9j. Salutogenic Design and Facility Procurement
1. Site Context + Spatial Organization
1a. Proximity to Infrastructure
Isolation is a serious concern for a relocated senior after residing in the old neighborhood for years if not decades. Relocation to a LTC home often severs friendships and social ties built over a long time—sewing clubs, bingo nights, church outings, bowling leagues, neighbors, Monday night recreational hockey and other sporting events, weekly dinners, shopping, day excursions with the grandchildren, family vacations. It is important for the resident to continue to still feel a part of that prior everyday life to the extent possible. Proximity denotes closeness to stores, grocery market, bakery, pharmacy, hair salon, the barber; these familiar places are likely no longer within walkable distance or via transit even though many still-active seniors remain familiar with their local public transit system.
Gerontological research shoes that residents miss the daily routines they took for granted in their former community. Make the transition as seamless as possible, architecturally. Provide a porte cochere’ at the main entrance to protect from the elements in inclement weather. Sidewalks facilitate walking to the nearest transit stop. A transit stop is across from the main entrance at the The Priory at Heritage Woods in Victoria, British Columbia. Residents can also walk to a civic square park two blocks away, and the commercial district and public library are a mere two blocks beyond. An accessible town center fosters connectedness. When walking becomes unfeasible, the wheelchair-access van will be deployed on a scheduled basis for excursions to destination points, including perhaps the nearby shopping mall, post office, and movie theatre. This vital proxemic link to the normative activities of daily living is too often unattainable in rural in other low-density locales. 1c; 6c; 9a; 9b; 9d
References:
1a-1. Rijnaard, M.D., Van Hoof, J., Janssen, B.M., Verbeek, H., Pocornie, W., Eijkelenboom, A., Beerens, H.C., Molony, S.L., & Wouters, E.J.M. (2016). The factors influencing the sense of home in nursing homes: A systematic review from the perspective of residents. Journal of Aging Research, 6143645. (PDF)
1a-2. Van Hoof, J., Verhagen, M. M., Wouters, E. J. M., Marston, H. R., Rijnaard, M. D., & Janssen, B. M. (2015). Picture your nursing home: Exploring the sense of home of older residents through photography. Journal of Aging Research, 312931. (PDF)
1b. Maximize Parti’ Logic
The largest LTC institutions in Ontario are the result of Provincial and care provider organizational policies that minimize capital construction costs per bed. Pressures continue in and beyond the coronovirus pandemic to over-concentrate beds per site. Instead of a 60 or 100 bed facility, often, facilities are still being programmed for up to 400 beds on a single site. This may be justifiable on a cost accounting basis, especially in light of continually accelerating land values, but in terms of quality of life it can result in a stultifying existence. The enormity of institutions of this magnitude of scale make them difficult to cognitively comprehend let alone navigate and actually enjoy on a daily basis. Quality of life suffers as a result. Oversized LTC facilities further exacerbate negative aspects of the multiple sensory deficits experienced by the aged. These include hearing loss, visual acuity decrements and a diminished range pf physical mobility. For the resident suffering from cognitive impairment, overscaled physical environments can become a threat.
The resident may shut down—exhibiting a form of learned helplessness. The built environment becomes too pressing for effective coping. This is what the pioneering environmental gerontologist M. Powell Lawton referred to in his environmental press-competency theory. The effort required for navigational mastery is outstripped by the sheer resistance, or press, posed by a physical setting. The problem usually begins with the functional brief. Instead of 300 beds, program 60, 75, 100 maximum. This scale-down process can foster human-scaled physical environments—environments inherently less pressing to navigate and master. Architectural legibility denotes conceptual comprehensibility. Comprehensibility needs among the aged in LTC home settings is greatest among residents with dementia and Alzheimer's and the percentage of residents with severe cognitive impairment is skyrocketing. Design to maximize executive cognitive functioning. Compositionally confusing (overly pressing) physical environments exacerbate residents’ cognitive disorientation, foster agitation, and result in physical and social withdrawal because the resident's personal coping (degree of competency) has been exceeded. 1c; 1d; 1e; 1f; 4c; 4g; 8b
References:
1b-1. Lawton, M.P. (1985). The elderly in context: Perspectives from environmental psychology and gerontology. Environment and Behavior, 17(4): 501-519.*
1b-2. Chaudhury, H., & Cooke, H. (2014). Design matters in dementia care: The role of the physical environment in dementia care settings. In M. Downs & B. Bowers (eds.), Excellence in Dementia Care (2nd ed.). Oxford: UK: Open University Press, 144-158. (PDF)
1b-3. Craig, C. (2017). Imagined futures: Designing future environments for the care of older people. The Design Journal, 20(1), S2336–S2347. (PDF)
1b-4. Orfield, S. (2015). Dementia environment design in seniors housing: Optimizing resident perception and cognition. Seniors Housing and Care Journal, 23(2), 58-69. (PDF)
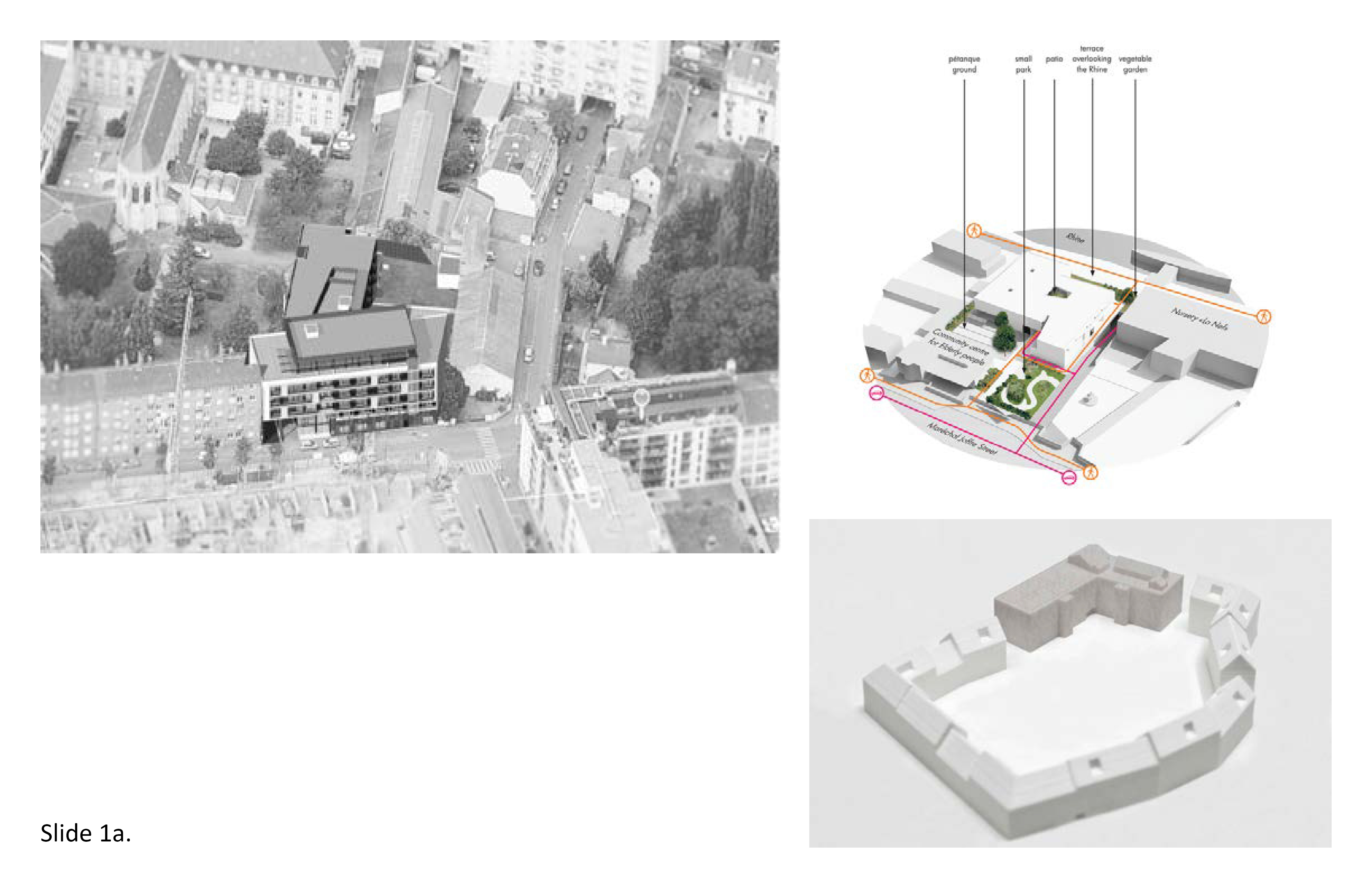
1c. Mixed-Use Campus
Long-term care residences need not be islands physically disconnected from everyday life. Geographically isolated LTC homes will need to overcompensate in this regard, providing the resident options to be transited off-site to obtain healthcare checkups, intergenerational contact with family and friends, shopping, religious worship, and so on. But opportunities also exist to locate LTC homes in places where it makes equal sense to combine the LTC home with one or more compatible mixed-use functions on the same site. This strategy will support activities of daily living (ADLs) of mutual benefit—benefitting the larger community while also benefitting the quality of daily LTC residential life. Why not bring ADLs and services to the resident that once were exclusively located off-site due to zoning or other restrictions? The status quo is obsolete. A higher degree of integration with the local community is achievable though compatible mixed-uses on the same site—educational (taking a university course onsite), medical (pharmacy), fiscal (bank) or a dining establishment (restaurant or café) to name but a few possible tenants.
Mixed-use LTC campuses are mutually beneficial if inventively planned and built. Explore mixed-use opportunities on-site from the earliest phases of site selection and facility planning. Care provider organizations will need to reach out to potential partners early on to achieve a mixed-use campus through this type of transprogrammation. Think not only of the primary building use but also other compatible services on-site—an optometry clinic, primary care clinic, eldercare day program for the neighborhood, small grocery, social services (mental health), and recreational amenities such as a public park or parkette. The architectural team can help brainstorm in attracting potential compatible tenants. These tenants can be housed on the ground level of a multi-level facility, or in a connected wing. To achieve genuine interconnectivity orient these mixed-use amenities for maximum acceptance and use by the local community. Urban case studies presented in Part I describe how a first floor can compatibly accommodate non-LTC tenants as well as open access public spaces. 1c; 1e; 5e; 6c; 9a; 9b

References:
1c-1. Aung, M., Koyanagi, Y., Ueno, S., Tiraphat, S., & Yuasa, M. (2021) A Contemporary insight into an age-friendly environments contributing to the social network, active ageing and quality of life of community resident seniors in Japan. Journal of Aging and Environment, 35(2), 145-160. (PDF)
1c-2. Jenkens, R., Thomas, W., & Barber, V. (2012). Can community-based services thrive in a licensed nursing home? Generations: Journal of the American Society on Aging, 36(1), 125-130. Retrieved May 21, 2021, from http://www.jstor.org/stable/44875748. (PDF)
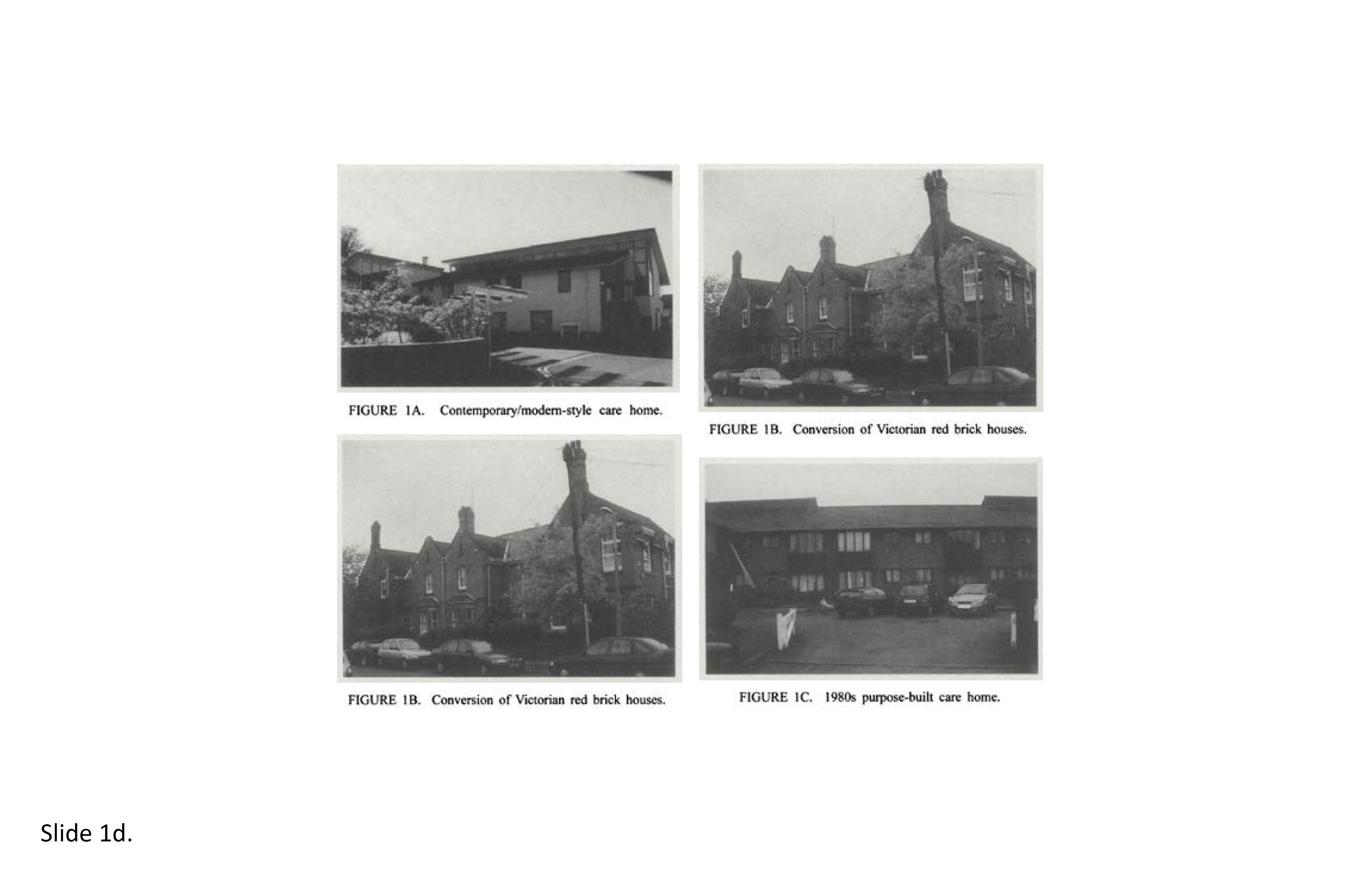
1d. Elderesidence Imagery
In the twentieth century, most Canadian seniors lived in intergenerational households under the same roof with children, grandchildren, pets, and extended family members. Architectural appearance was important but style per se was no more important than functionality, adaptability, and physical proximity to meaningful amenities in the immediate neighborhood, town and region. In the early twentieth century, preferred Canadian residential architecture was highly influenced by British private upper-class residences such as those designed by Edwyn Lutyens, Charles Rennie Mackintosh, and their contemporaries. Post-WWII, the correct image for the progressive, medically-based nursing home became International Style modernism—no ornamentation, flat roofs, monochromicity—an overall minimalist aesthetic. However, the majority of aged did not accept minimalism. This was underscored in a recent evidence-based study of preferred residential imagery among the aged, with traditional residential imagery more preferred than minimalist architectural vocabularies (1d-4).
While architectural style is important it cannot override functionality, invitingness, and adaptability. Amenities needed in everyday life include windows that provide views of interest without sacrificing personal privacy within the dwelling, typologies that draw from vernacular building methods and aesthetic vocabularies, local materiality, color palettes, appropriate scale, and compositional massing, and neighborhood layout. Prior, most seniors lived in private residences, or apartments four levels in height or less; it stands to reason they still prefer to live in similar (low-rise) buildings. For an 87-year old male and his 85-rear old spouse, who lived for decades in a suburban ranch in Etobicoke, Ontario, relocation to an upper floor of a “contemporary” high-rise LTC facility in Brampton is disruptive, dislocational. Newly constructed LTC residences should be no more than four or five levels in height and express a residential or quasi-residential image. 1b; 1f; 3a; 5d; 6d; 7b; 8a
References:
1d-1. Andersson, Granath, K., & Nylander, O. (2021). Aging-in-place: Residents’ attitudes and floor plan potential in apartment buildings from 1990 to 2015. Health Environments Research & Design Journal, 14(4), 211–226. (PDF)
1d-2. Burton, E., & Sheehan, B. (2010). Care-home environments and well-being: Identifying the design features that most affect older residents. Journal of Architectural and Planning Research, 27(3), 241-242. (PDF)
1d-3. Boydell, K. (2014). Best Practice In Housing Design For Seniors' Supportive Housing. Waterloo: Ontario: Regional Municipality Of Waterloo. (PDF)
1d-4. Cerina, V. Fornara, F., & Manica, S. (2017). Architectural style and green spaces predict older adults’ evaluations of residential facilities. European Journal of Ageing, 14(3), 207-217. (PDF)
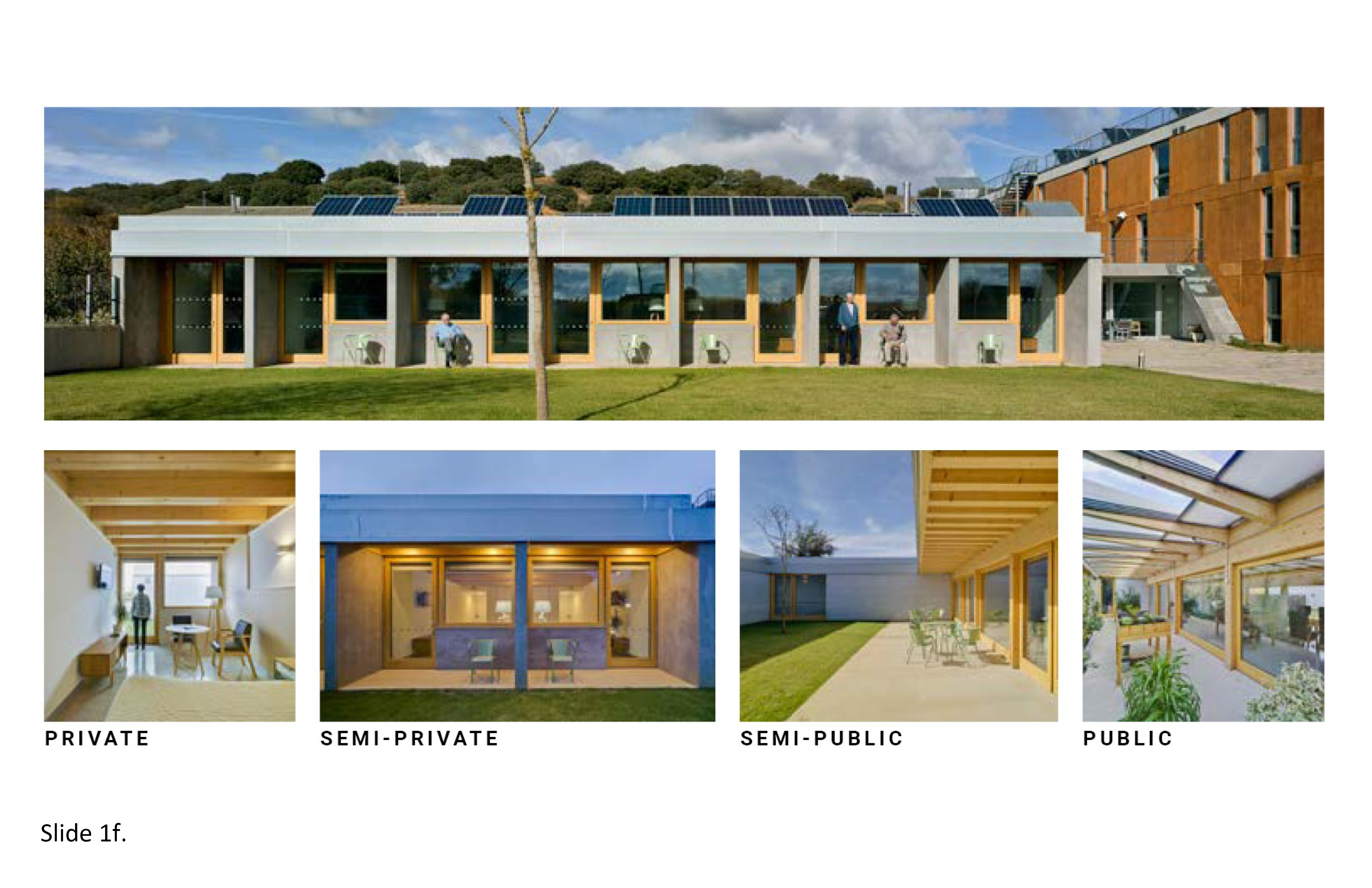
1e. Hierarchical Realms
Most nursing homes constructed in Canada the 1960s and 1970s were hierarchically deficient, their facades slamming to the ground like guillotines, as if to physically isolate their occupants. By contrast, private dwellings typically express four spatial zones—public, semi-public, semi-private, and private—with each zone seldom functioning as mutually exclusive of of the others. Natural overlaps and functional spillovers randomly occur, i.e. when the teenage son practices playing the saxophone every afternoon from 4:00-6:00pm, thereby “taking over” virtually the entire residential zone for the duration of that activity. The four zones endure cross-culturally across time and space, adaptable to the expression of diverse cultural norms and traditions. For the aged household member, this is relevant both in theory and practice. When applied to the LTC milieu, the built environment needs to diversely accommodate hierarchical fluidity in support of ADLs and associated activities. Specific rooms devoted for quiet time, socialization, personal hygiene, food preparation and dining, intimacy, are examples while other spaces should accommodate multiple uses, perhaps concurrently.
In LTC residences, spaces for socialization too often are dysfunctional, expressing distorted, convoluted hierarchical adjacencies. At worst, architecturally, one or two of the aforementioned zones may be entirely unsupported. A kitchen without a countertop for casual dining options, or a dining room without an exterior patio allowing for outdoor dining as weather permits, pose unwarranted physical and psychosocial barriers. A wandering garden too small signifies excessive, problemmatic, spatial compression. Shortcomings of this type are traceable to site selection. The site is undersized, poorly located, due to a flawed functional brief. As but one example of this syndrome, communal spaces such as kitchens and dining areas facilitate strong connectivity between hierarchical realms and afford opportunities for all to congregate. Exterior spaces such as courtyards and side yards, balconies, and roof terraces also support this strategy. It is about non-repetitiveness, anti-institutionalism and, alternatively, residentialism. 1b; 1f; 3b; 4d; 4g; 7b

References:
1e-1.Cohen, L. W., Zimmerman, S., Reed, D., Brown, P. B., Bowers, B. J., Nolet, K., Hudak, S. L., & Horn, S. D. (2016). The green house model of nursing home care in design and practice. Health Services Research, 51(1), 352–377. (PDF)
1e-2. Wrublowsky, R. (2018). Design Guide for Long Term Care Homes. MMP Architects. (PDF)
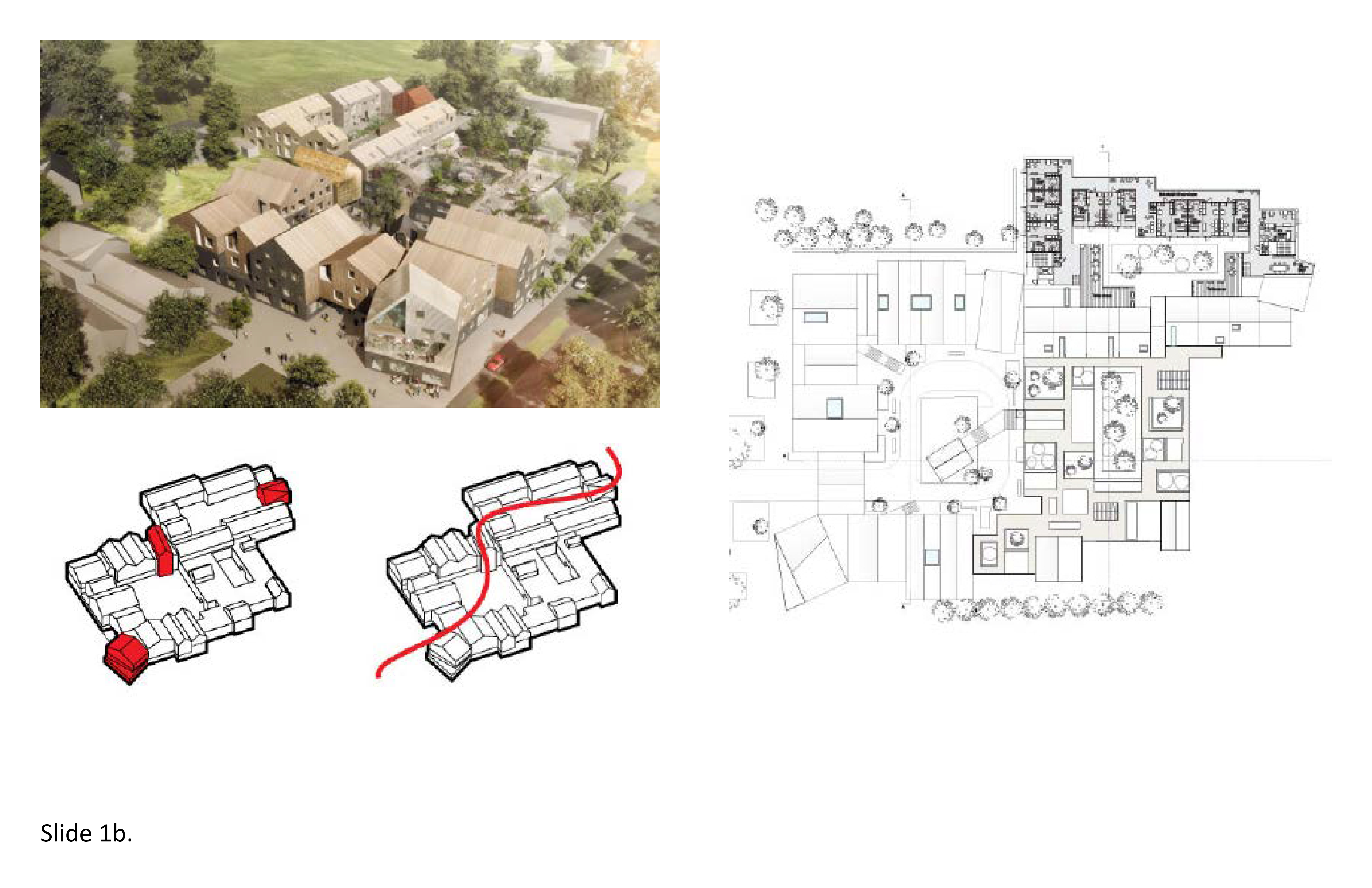
1f. Decentralized Houses
Today's megahospitals result from decades-long efforts to over-concentrate capital investments in the fewest number of buildings and to maximize the bed counts and related medical services on highly centralized sites. These same policies generally drove LTC home construction in Ontario. In the case of the LTC industry, policies that once may have been easily rationalized now warrant thorough reappraisal. The bigger-is-better philosophy fell far short. This resulted in overcrowded LTC residences with too many beds per site and too many beds per bedroom. The oldest facilities still in operation are depersonalizing, at worst, dehumanizing for the resident. This is not to argue for eldercare residences of no more than 50 or 75 beds per site. Rather, multiple interconnected clusters can be inventively created with each "house" or unit projecting a residential image.
Multiple semi-autonomous houses of 10-15 residents maximum provide opportunities to establish decentralization, appropriate architectural scale, campus imagery, and a sense of place. For the resident, clustering strategies allow for individualized private and semi-private in-between zones. Each house or unit autonomously supports a range of ADLs, engagement with the outdoors, nutritional health, socialization and privacy needs, and therapy regimens. Within each house, organize the four aforementioned spatial zones to function as loci of activity, i.e. personal hygiene, dayrooms, decentralized dining options, access to the outdoors, outdoor amenities and related indoor semi-private and private space. Design the house so residents and staff can visit other houses without having to walk through the main lobby. The Green House model of long-term care is premised on this concept and is appropriate for low-rise as well as mid-rise LTC applications. Houses on the upper floors of mid-ride facilities can achieve these same qualities by means of roof terraces, connector walkways, and balconies. 1b; 1d; 1e; 2c; 3b; 4d; 5c
References:
1f-1. Anderson, D. C., Grey, T., Kennelly, S., & O'Neill, D. (2020). Nursing home design and COVID-19: Balancing infection control, quality of life, and resilience. Journal of the American Medical Directors Association, 21(11), 1519–1524. (PDF)
1f-2. Cohen, L. W., Zimmerman, S., Reed, D., Brown, P. B., Bowers, B. J., Nolet, K., Hudak, S. L., & Horn, S. D. (2016). The green house model of nursing home care in design and practice. Health Services Research, 51(1), 352–377. (PDF)
1f-3. De Rooij, A. H., Luijkx, K. G., Schaafsma, J., Declercq, A. G., Emmerink, P. M., & Schols, J. M. (2012). Quality of life of residents with dementia in traditional versus small-scale long-term care settings: A Quasi-Experimental Study. International Journal Of Nursing Studies, 49(8), 931–940. (PDF)
1f-4. Wrublowsky, R. (2018) Design Guide for Long Term Care Homes. MMP Architects. (PDF)
2. Private Realm
2a. Medically Safe Bedrooms
The Covid-19 pandemic rendered the bedroom/hygiene zone in LTC residences medically unsafe from an infection control standpoint. This became evident early on due to disproportionately high mortality rates in LTC facilities. A deadly pattern emerged in 2020 that persisted, often due to bedroom overcrowding, insufficient space for personal distancing, and hygiene needs. The 2 to 4-bed semi-private bedroom model was a lingering artifact from the 1960s and 1970s nursing home, where, because it was then acceptable to house hospitalized patients in an open hospital ward--it was rationalized this same practice would suffice in institutionally housing the aged. Covid-19 proved the fallacy of this practice once and for all. Not only were communal sleeping and personal hygiene accommodations a hazardous prescription, it was also a hazardous policy for the caregiver staff. Caregivers were subject to these overcrowded conditions, fostering viral transmissions as a result. Antiquated HVAC and natural ventilation levels only made matters worse.
Under intense media scrutiny, LTC provider organizations were suddenly under intense pressure to retrofit their facilities yesterday. But this was often impossible due to the intractably rigid architecture of these facilities—particularly those built prior to 1990. Major facility retrofits on-site were unfeasible in the midst of the pandemic, and the overnight creation of all private bedrooms was ruled out (financially) because it would lower occupancy without yielding scientifically proven positive health outcomes. Nonetheless, it is now widely assumed the best practice in long-term residence planning and design is a small-scale, all-private bedroom configuration with in-room private bath-shower. The recent medical literature clearly supports this practice. For the architect, the question now is how to best renovate semi-private configurations in existing facilities, and how to inventively design newly-built, medically safe all-private bedroom facilities in smaller-scaled LTC residential settings. 1f; 2c; 3b; 4f; 5e; 7e; 9c

References:
2a-1. Agarwal, M., Stone, P. W., & Dick, A. (2019). Evaluation of nursing home infection control programs: A pre-and post-study. American Journal of Infection Control, 47(6), S34–S34. (PDF)
2a-2. Anderson, D. C., Grey, T., Kennelly, S., & O'Neill, D. (2020). Nursing home design and COVID-19: Balancing infection control, quality of life, and resilience. Journal of the American Medical Directors Association, 21(11), 1519–1524. (PDF)
2a-3. Brown, K. A., Jones, A., Daneman, N., Chan, A. K., Schwartz, K. L., Garber, G. E., Costa, A. P., & Stall, N. M. (2021). Association between nursing home crowding and COVID-19 infection and mortality in Ontario, Canada. JAMA Internal Medicine, 181(2), 229–236. (PDF)
2a-4. Calkins, M., & Cassella, C. (2007). Exploring the cost and value of private versus shared bedrooms in nursing homes. The Gerontologist, 47(2), 169–183. (PDF)
2a-5. Chaudhury, H., Cooke, H. A., Cowie, H., & Razaghi, L. (2018). The influence of the physical environment on residents with dementia in long-term care settings: A review of the empirical literature. The Gerontologist, 58(5), 325-337. (PDF)
2a-6. Gordon, A. ., Goodman, C., Achterberg, W., Barker, R. ., Burns, E., Hanratty, B., Martin, F., Meyer, J., O’Neill, D., Schols, J., & Spilsbury, K. (2020). Commentary: COVID in care homes-challenges and dilemmas in healthcare delivery. Age and Ageing, 49(5), 701–705. (PDF)
2a-7. Stone, P. W., Herzig, C. T. ., Pogorzelska-Maziarz, M., Carter, E., Bjarnadottir, R. I., Semeraro, P. K., Cohen, C. C., Travers, J., & Schweon, S. (2015). Understanding infection prevention and control in nursing homes: A qualitative study. Geriatric Nursing (New York), 36(4), 267–272. (PDF)
2b. Balconies and Patios
The exterior spaces on elderesidence campuses can foster prospect-refuge behaviors ranging from quiet contemplation to various social activities. Their therapeutic affordances support the predilections of residents, visitors, and caregiver staff in seeking breaks from monotonous, understimulating conditions indoors. An outdoor “room” of this type—whether a central courtyard, decentralized pockets of seating, a protected wandering garden—are places where one can obtain respite—fostering involuntary attentional stimulation, in accord with Attention Restoration Theory. A private balcony adjacent to every bedroom or pair of bedrooms, or an open continuous terrace, function as an extensions of the interior realm in providing respite. Their exteriorality expands the room into the external world while at the same time providing a place to get away without actually leaving the facility. This is especially important in the case of small bedrooms. Spatial expansiveness obtained through engagement with nature simultaneously functions to transmit daylight and natural ventilation into the interior.
A private balcony can allow for solace, contemplation, and personal autonomy, for the resident to use as desired as the weather allows. A balcony inset into the building envelope such as at the Wilder Kaiser Nursing Home in Austria (2017), illustrates how the building envelope can provide protection from the elements, its physical depth allowing for a table and chairs. These spaces are, in effect, external rooms. Balconies too narrow for this type of use are useless. Neither should a balcony or terrace make the resident and family/friends feel unsafe or visually overexposed. If the balcony extends outward from the envelope, provide a roof or canopy for at least partial protection, or privacy panels between balconies along continuous exterior spaces. In the case of ground level patios, visual privacy is equally important. Visually screen the ground-level patios with landscaping, a trellis, and non-institutional perimeter walls and fences. See Part I for case study examples of successful balconies and patios in LTC built environments. 1d; 1f; 4f; 6a; 7b; 7c; 9d

References:
2b-1. Bengtsson, A., Hägerhäll, C., Englund, J.-E., & Grahn, P. (2015). Outdoor Environments at Three Nursing Homes: Semantic Environmental Descriptions. Journal of Housing for the Elderly, 29(1-2), 53-76. (PDF)
2b-2. Rijnaard, M.D., Van Hoof, J., Janssen, B.M., Verbeek, H., Pocornie, W., Eijkelenboom, A., Beerens, H.C., Molony, S.L., & Wouters, E.J.M. (2016). The factors influencing the sense of home in nursing homes: A systematic review from the perspective of residents. Journal of Aging Research, 13(2), 6143645. (PDF)
2b-3. Vecellio, D. J., Bardenhagen, E. K., Lerman, B., & Brown, R. D. (2021). The role of outdoor microclimatic features at long-term care facilities in advancing the health of its residents: An integrative review and future strategies. Environmental Research, 201, 111583–111583. (PDF)
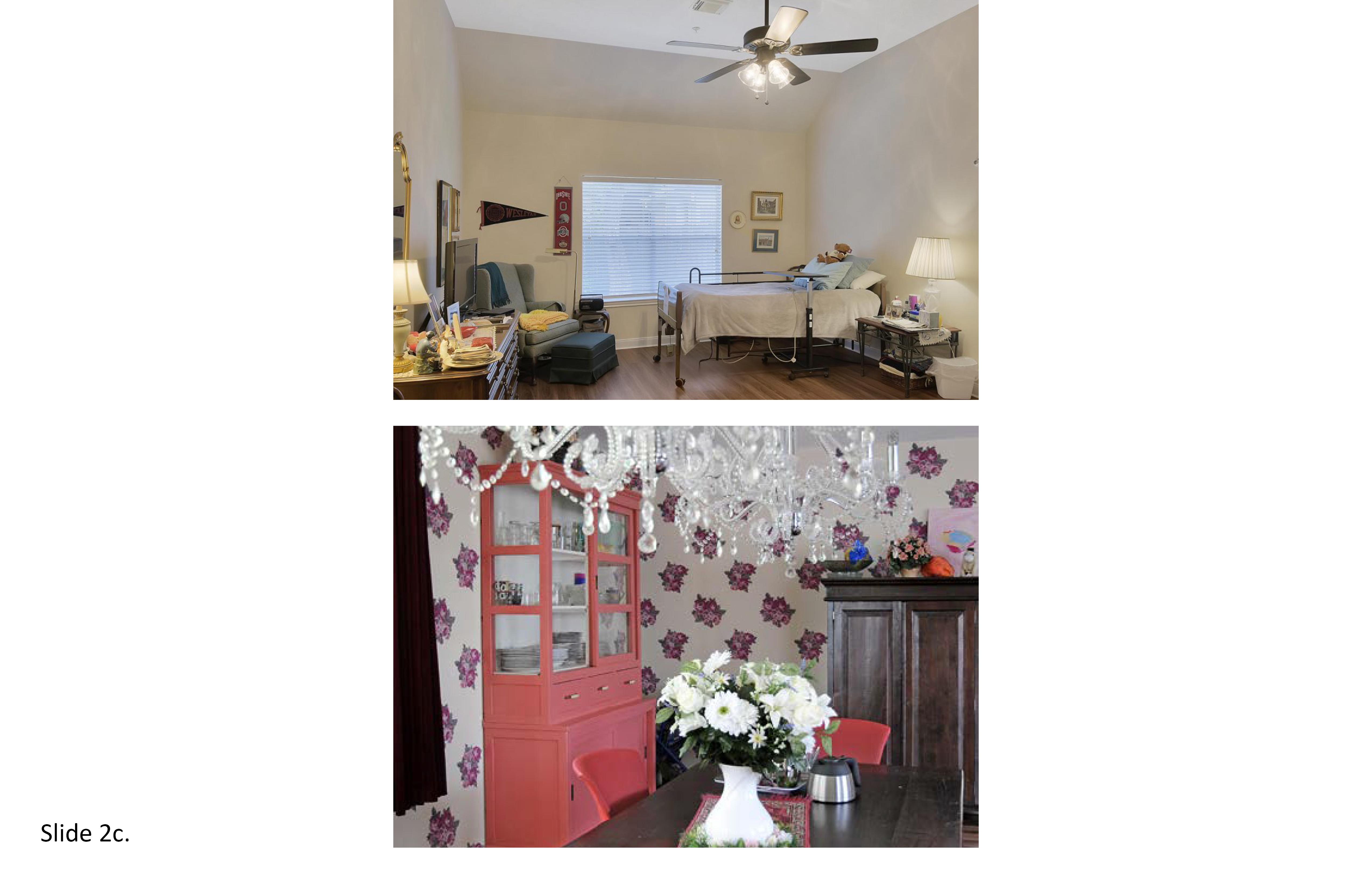
2c. Personalization and Distancing
The modern nursing home took its architectural cues from the acute care modern hospital. Many hospitals' minimalist aesthetic, institutionalism, centralization of medical services, harsh materials of construction, and massive scale had a dehumanizing effect. Building codes and minimum construction standards for nursing homes were patterned on those of these hospitals. The inpatient geriatric units housed in acute care institutions were exported into the nursing home, with predictable results. Architecturally, the nursing home was uninspiring with little regard for the personal dignity or past life experiences of the "invalid" skilled nursing care patient. Institutional policies often disallowed the family from personalizing the bedroom—because it was shared with other patients—thereby further underscoring the aesthetic of a hospital room. In the extreme, it was little more than a new type of institution, similarly intended for temporary occupancy.
Innovative policies are needed in support of self-actualization, personalization, and dignity. Personal distancing (all-private bedrooms, and sufficiently spacious communal spaces), together with the spatial personalization of the private zone of the bedroom, are appropriate. Take measures to foster the resident's sense of self-control, personal identity, and the conveyance of life experiences; other residents (and staff) should be able to view and learn about one’s life including photos of one's loved ones. This can be something as simple as the provision of memory boxes in the threshold-entry zone, larger bedrooms, socialization spaces, and wider corridors, allowing for chairs, side tables and built-in window seats. Inside the bedroom, provide places for plants, artwork and space for a rug, bed and perahps a side dresser from one’s prior dwelling. These measures contribute to a deinstitutionalized atmosphere, innovations pioneered decades ago in Scandinavian long-term care residences. For the resident and family, greater room personalization and personal distancing in LTC homes will result in a higher level of satisfaction with the overall built environment. 1e; 4d; 5b; 5c; 5e
References:
2c-1. Chaudhury, H., Cooke, H. A., Cowie, H., & Razaghi, L. (2018). The influence of the physical environment on residents with dementia in long-term care settings: A review of the empirical literature. The Gerontologist, 58(5), 325-337. (PDF)
2c-2. Chu, C. H., Donato‐Woodger, S., & Dainton, C. J. (2020). Competing crises: COVID‐19 countermeasures and social isolation among older adults in long‐term care. Journal of Advanced Nursing, 76(10), 2456–2459. (PDF)
2c-3. Fleming, R., & Purandare, N. (2010). Long-term care for people with dementia: environmental design guidelines. International Psychogeriatrics, 22(2), 1084–1096. (PDF)
2c-4. Gale, A. & Park, N.-K. (2010) Desired and achieved privacy and interaction in multigenerational homes, Housing and Society, 37(1), pp. 25–41. (PDF)
2c-5. Van Hoof, J., Janssen, M. L., Heesakkers, C. M. C., van Kersbergen, W., Severijns, L. E. J., Willems, L. A. G., Marston, H. R., Janssen, B. M., & Nieboer, M. E. (2016). The importance of personal possessions for the development of a sense of home in nursing home residents. Journal of Housing for the Elderly, 30(1), 35–51. (PDF)
2d. Universal Washrooms
The coronavirus pandemic fueled a complete reassessment of personal hygiene and personal distancing. Communal personal hygiene spaces are oxymoronic: they proved ideal as hosts for the transmission of infectious disease. Restated, the semi-private bedroom and semi-private washroom-shower unit are high-probability infectious disease transmitters. Residences with two more occupants sharing the same bedroom and washroom-shower unit are infectious disease transmitters. Alternatively, provide all-private bedrooms with private washroom-shower unit. This is predicted to yield lower infectious disease transmission rates while allowing for improved privacy in the personal hygiene experience. This will likely result in additional staff required, as more individualization often requires additional staff attentiveness. Despite the cost ramifications of greater personalization and functional universality, these design and equipment standards will elevate the resident’s medical safety, sense of self-dignity, control, and autonomy--outcomes that align with greater infection control and personal distancing.
Universal Design (UD) is standard practice across the healthcare industry. It applies to exterior as much as interior environments and is premised on the principle of non-discrimination in design and associated technological support. A resident should not be prohibited or discouraged from effectively using any space or amenity, especially fixtures and equipment designed to promote personal hygiene. Universal washroom-shower rooms must support a broad range of physical mobility, sensory and cognitive abilities, i.e. providing an equal space on both sides of the toilet in support of multiple transfer methods. If possible, position the toilet in the direct line of sight from the bed; employ varied colors on wall surfaces, with differentiated visual cues to help promote their heightened legibility. Bath-shower units can be difficult to negotiate in the best of circumstances and their sensory legibility and physical properties can be further enhanced with a window (with obscured glass). 1f; 2a; 2c; 3b; 5e; 7a

References:
2d-1. Boge, J., Callewaert, S., & Petersen, K. A. (2017). The impact of bathroom design on privacy for users with special needs. Ageing International, 44(3), 300–317. (PDF)
2d-2. Cohen, L. W., Zimmerman, S., Reed, D., Brown, P. B., Bowers, B. J., Nolet, K., Hudak, S. L., & Horn, S. D. (2016). The green house model of nursing home care in design and practice. Health Services Research, 51(1), 352–377. (PDF)
2d-3. Steeves, J. (2005). Examination of Universal Design in Kitchens and Bathrooms of the Housing and Urban Development Demonstration Program: Elderly Cottage Housing. Washington, DC: Department of Housing and Urban Development. opportunity. (PDF)
2d-4. Wrublowsky, R. (2018) Design Guide for Long Term Care Homes. MMP Architects. (PDF)
3. Shared Realm
3a. Kitchens and Dining Areas
Ideally, the aged are best served through in-home care supports that allow the individual to remain out of institutional LTC for as long as possible. This model, however, is premised on community-based eldercare organizations in place locally to provide home healthcare support. In communities where these supports are well established the result should be that only those most in need of long-term care will ever be relocated to a 24/7 residential setting. When one becomes unable to maintain ADLs—personal hygiene, food preparation, home maintenance, personal finances and so on, independent living becomes impossible. An individual may still be able to provide simple meals for oneself, particularly meals not requiring a conventional oven. But this is temporary— for cooking out of a microwave because one has forgotten how to use the oven is dangerous. In LTC homes a central kitchen and multiple eating options safely support nutritional health needs, and ideally, freedom to self-select where one eats, when, and with whom.
The kitchen should be designed for visitors to self-prepare a meal, or the resident him-herself, if functionally capable, safety, without risk to others. Provide enough dining tables so more than one family can dine simultaneously yet independently. Design a countertop eating area, and all furnishings for wheelchair access. Provide for food storage in one (or two) refrigerators, a double-compartment sink (ideally, next to an exterior window), microwave, dishwasher, cabinets, and pantry. Locate the kitchen and dining area at the heart of the unit/house next to a roof terrace or patio with a canopy or extended roof eave. Establish the aesthetic, ambiance, and functionality of a residential kitchen. This contributes to a universal, normative residential image. Accommodate up to twelve residents at once with family style dining tables, artwork, and full height windows. Many excellent recent case study precedents exist in Europe (Part I). 1e; 3b; 3c; 5a; 6a; 7b

References:
3a-1. Calkins, M. P. (2009). Evidence-based long term care design. NeuroRehabilitation, 25(3), 151-152. (PDF)
3a-2. Chaudhury, H., Hung, L., & Badger, M. (2013). The role of physical environment in supporting person-centered dining in long-term care: a review of the literature. American Journal of Alzheimer’s Disease and Other Dementias, 28(2), 492-500. (PDF)
3a-3. Chaudhury, H., Hung, L., Rust, T., & Wu, S. (2016). Do physical environmental changes make a difference? Supporting person-centered care at mealtimes in nursing homes. Dementia: The International Journal of Social Research and Practice, 14(2), 879-896. (PDF)
3a-4. van Hoof, J., Wetzels, M., Dooremalen, A. M., Wouters, E. J., Nieboer, et al. (2014). Technological and architectural solutions for Dutch nursing homes: Results of a multidisciplinary mind mapping session with professional stakeholders. Technology in Society, 36(1), 1–12. (PDF)
3b. Prospect-Refuge Imperatives
In LTC homes, territorial autonomy is a fundamental design consideration. Midsize to large-size facilities are least supportive in this regard mainly due to programmatic compression and the resulting spatial compression has a direct influence on residents' patterns of behavior. The over-compression of spaces for social interaction, therapy, and informal places for residents to simply hang out is a main contributor to the institutionalism of many LTC homes. Personal space for use by residents and for visitations by family members and friends provides the freedom of choice to self-determine if adequate prospect (socialization)/refuge (privacy) activities are obtainable, where, and when. The prospect/refuge construct also applies to staff personnel. For the resident, however, spatial over-compression potentially suppresses wandering behaviors—a prospect/refuge physical activity encouraged in memory care units. The lack of adequate space for decompression (and also staff) begins with site selection: an overly compact site will result in an excessively compressed building footprint and/or a building too tall.
Prospect/Refuge: Select a site that allows interconnected, semi-autonomous structures. Terraces, patios, walkways, connecting footbridges facilitate freedom to circulate within spatial limits. Provide interior and exterior paths and points of destination that prompt exploration and prospect/refuge territorial imperatives within the confines of a safe, protected physical setting. Foster congruences between the built environment and the social-behavioral environment. Provide seating and places to stop, rest or converse along circulation paths. Coordinate these nodes with the four aforementioned spatial zones to ensure they do not inadvertently intersect, impede, or diminish the function of any individual node or zone. Memory care residents will particularly benefit, physically and cognitively from the option to experience more, beyond the four walls of a single building or their own residential unit/house. 1e; 4d; 5a; 5e; 6a; 7b

References:
3b-1. Campo, M., & Chaudhury, H. (2012). Informal social interaction among residents with dementia in special care units: Exploring the role of the physical and social environments. Dementia: The International Journal of Social Research and Practice, 11(2), 401–423. (PDF)
3b-2. Ferdous, F. (2021). Redesigning memory care in the COVID-19 era: Interdisciplinary spatial design interventions to minimize social isolation in older adults. Journal of Aging & Social Policy, 33(4-5), 555–569. (PDF)
3b-3. Verbeek, H., van Rossum, E., Zwakhalen, S., M.Kempen, G. I., & Hamers, J. P. (2009). Small, homelike care environments for older people with dementia: A literature review. International Psychogeriatrics, 21(3), 252–264. (PDF)
3c. Foster Everyday Activities
Medical safety is of utmost priority in planning and designing 24/7 care facilities for the aged. This lesson was learned the hard way in the early days of the coronavirus pandemic. LTC residences that allowed for adequate social distancing helped mitigate the transmission of infectious disease. However, from a therapeutic and socialization perspective, this should be achieved without disengaging the resident from normative activities of everyday life. It is important to be out and about during the day as deemed safe and appropriate by the caregiver team. This requires designing for an array of activities of everyday living whereby the resident is able to meaningfully engage in therapeutic treatment, physical activity, social engagement, and the biophilic affordances of engagement with nature and landscape. Everyday activities range from watching a film in the dayroom, physical therapy, being outdoors in one’s wheelchair in the wandering garden, and being transited offsite for special excursions.
The aged in institutional care settings are subject to elder-abuse including acts of negligence, and hostile acts perpetuated by unprofessional, dismissive staff who depersonalize—dehumanize—those for whom they are paid to care for. Benign neglect and physical abuse must be replaced by life-affirming ADLs that include social activities, films, watching the news on television, music events, passing the time with visitors, being outdoors on a nice day, excursions off campus for shopping, dining, a concert at the nearby park and in general engaging in activities of everyday life that continue to be intrinsically enjoyable—positive distractions from one’s daily routine. Ask the resident this question, “What activities of daily living are still considered of interest to you?” The activities listed generally will not include prescribed medical treatment, i.e. PT. Instead, art therapy, horticultural and recreational therapy, spending time in the multisensory room, a pet therapy session, or perhaps in occupational therapy. 1a; 1c; 3d; 4a; 4c; 5a; 5e

References:
3c-1. Campo, M., & Chaudhury, H. (2012). Informal social interaction among residents with dementia in special care units: Exploring the role of the physical and social environments. Dementia: The International Journal of Social Research and Practice, 11(2), 401–423. (PDF)
3c-2. Nasrallah, E., & Pati, D. (2021). Can physical design help reduce loneliness in the elderly? A theoretical exploration. Health Environments Research & Design Journal, 14(3), 374–385. (PDF)
3c-3. Verbeek, H., van Rossum, E., Zwakhalen, S., M.Kempen, G. I., & Hamers, J. P. (2009). Small, homelike care environments for older people with dementia: A literature review. International Psychogeriatrics, 21(3), 252–264. (PDF)
3d. Functional Adaptation
The programmatic (spatial) compression of the modern nursing home has became a dysfunctional aspect of older LTC facilities across Ontario--especially in light of the current movement to improve residents' engagement with nature and landscape as a means to preclude Nature-Deficit Disorder. The range of spaces provided in older facilities, often, now do not support the current range of ADL programs. The dayroom, for instance, was designed as a one-size-fits all room to support a broad range of functions from counseling sessions to visitations with family and friends, to dining and recreational activities. They were over-programmed and often undersized, and lacked meaningful connections with nature and landscape. Dayrooms were an outgrowth of the minimalism of the modern acute care hospital, which provided a small visitor’s lounge at the end of the corridor, a cafeteria on the ground level, and little more. With the reinvention of long-term care facilities that commenced in the 1970s in Scandinavia the aim was to provide multiple informal, more adaptable activity rooms in support of a broader range of therapeutic, social, and recreational uses that also at times allow for activities to be scheduled, as needed, as well, by the local community.
From a quality of life standpoint it is preferable to provide interconnected, hierarchical networks of multipurpose activity rooms, some with higher ceilings than others, some with more horizontality, others smaller in size and more intimate, able to be partitioned into even smaller activity rooms with fold-away wall panels. This can foster social interaction more effectively than having to depend on one large multipurpose dayroom. Events can range from concerts, meetings, bingo nights, holiday celebrations to horticultural therapy events. Include a winter garden and greenhouses so these spaces can be used year-round. Provide multiple furnishing and seating options, reconfigurable furnishings, and a main living room with perhaps a fireplace, with warm inviting colors, materials, and a direct visual connection with the outdoors vis-à-vis full height windows, clerestories, skylights, and varied ceiling configurations. 2c; 3a; 3b; 3c; 4a; 6a; 6c

References:
3d-1. Boydell, K. (2014). Best Practice in Housing Design for Seniors’ Supportive Housing. Regional Municipality of Waterloo, 10-13.*
3d-2. Chaudhury, H., Cooke, H. A., Cowie, H., & Razaghi, L. (2018). The influence of the physical environment on residents with dementia in long-term care settings: A review of the empirical literature. The Gerontologist, 58(5), 325-337. (PDF)
3d-3. Rijnaard, M.D., Van Hoof, J., Janssen, B.M., Verbeek, H., Pocornie, W., Eijkelenboom, A., Beerens, H.C., Molony, S.L., & Wouters, E.J.M. (2016). The factors influencing the sense of home in nursing homes: A systematic review from the perspective of residents. Journal of Aging Research, 12(4), 6-11, 6143645. (PDF)
3d-4. Stevens, R., Petermans, A., Vanrie, J., & Van Cleempoel, K. (2013). Well-being from the perspective of interior architecture: Expected experience about residing in residential care centers. IASDR13, 4(1-2), 6-7. (PDF)
4. Biophilia—Nature Connectivity
4a. Age Appropriateness
Warehousing is a derogative term to describe how wealthy societies generally care for their aged. The term arose to describe the harsh, minimalist, unkempt nursing institutions of the past. Invalids were sent to these places not unlike shipping a person deemed in need of psychiatric treatment in the 19th century off to the nearest asylum. They were symbolically and literally places (and people) who were by default underfunded, misunderstood, undervalued. Few innovative architectural amenities were able to be provided because the construction budgets were insufficient. In thousands of high-rise nursing institutions seldom was the individual able to view a natural landscape from a balcony, smell the flowers, or feel the wind and sunshine outdoors in a beautiful garden. Walking is a preferred activity among the active elderly; it is a prime source of exercise, provides opportunities to socialize, and a psychological diversion—a positive distraction from one’s daily routine. Preferred age appropriate places for walking activity include parks, forests, neighborhoods with sidewalks, traditional town centers, such as Uxbridge, or Collingswood, Ontario, and suburban shopping malls of larger cities such as Toronto.
In urban contexts there is financial return-on-investment pressure to maximize (build out) the building’s height and footprint to an extent that disallows meaningful green space. Safe, age-appropriate roof terraces and gardens provide opportunities to be outdoors in proximity to residential supports. Age appropriate spaces are safe from an infection control perspective and provide protection from the elements. Memory care unit gardens and associated spaces must minimize transmission of infectious disease through social distancing. Provide shade and protection from the elements vis-à-vis canopied patios and roof terraces, protected by extended roof eaves or cantilevers. Provide seating, tables, places to sit, contemplate, or engage in social activity. Do not allow non-age appropriate activities such as games involving balls as this may cause injury to residents. 3c; 5e; 6a; 6c; 8c; 9d

References:
4a-1. Chi, P., Gutberg, J., & Berta, W. (2020). The conceptualization of the natural environment in healthcare facilities: A scoping review. Health Environments Research & Design Journal, 13(1), 30–47. (PDF)
4a-2. Hsieh, C.-H., Chen, C.-M., Yang, J.-Y., Lin, Y.-J., Liao, M.-L., & Chueh, K.-H. (2021). The effects of immersive garden experience on the health care of elderly residents with mild-to-moderate cognitive impairment living In nursing homes after the Covid-19 pandemic. Landscape And Ecological Engineering, 18(1), 45–56. (PDF)
4a-3. Peters, T., & Verderber, S. (2021). Biophilic design strategies in long-term residential care environments for persons with dementia. Journal of Aging and Environment, (PDF)
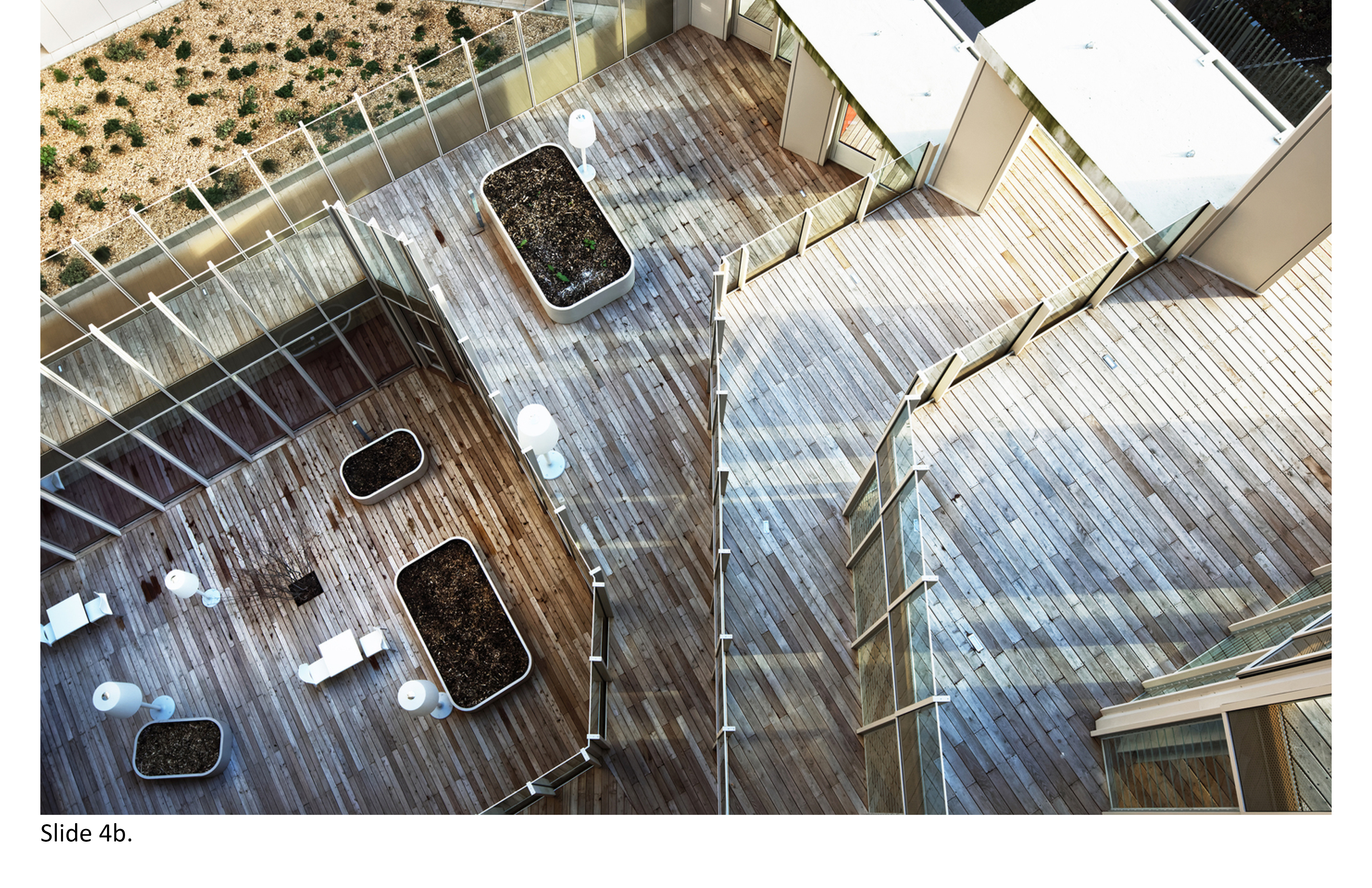
4b. Roof Terraces
The iconic Paimio Sanitorium (1929-1933) near Helsinki, Finland, designed by Alvar Aalto (born 1898-died 1976), featured expansive exterior terraces with plantings. This degree of person-nature connectivity in hospitals would be dismissed in the mega-medical centers of the 1960s and 1970s built across North America. Similarly, few nursing homes built in these years would feature anything quite like Paimio. The nursing home had become an internalized world onto itself. Taking its architectural cues from the acute care hospitals of the era, there were no balconies, terraces or similar amenities. The patient was therefore unable to experience sustained engagement with nature and landscape. The views might be of a parking lot, nearby building or light well—poor substitutes for a properly sized exterior courtyard and meaningful views of nature from indoors.
Biophilic and salutogenic, i.e. health-promoting (not pathology-based), design strategies warrant consideration in the establishing meaningful connectivity with nature, not merely episodically, but sustainably. Undulating stepped roof terraces and inset, projecting balconies, exterior furnishings, greenhouses, all-season winter gardens with sliding and retractable walls and roofs, or roll-up garage doors are feasible in this regard. Provide shade by means of canopies, trellises, extended roof eaves, shade trees, and related plantings to provide sufficient visual and acoustical privacy. It does little good to provide a roof terrace that is unbuffered from a noise control standpoint, i.e. an adjacent parking deck with cars coming and going at all hours. Establish a biophilic spatial hierarchy beginning at the ground level. In dense site contexts, horizontal and vertical green spaces and wall surfaces can be orchestrated whereby one or more stepped roof terraces are visually and spatially interconnected to bisecting vertical cutouts spanning from the ground level upward to the roof. 1e; 2b; 4c; 4d; 5e; 6c; 7f
References:
4b-1. Lee, E. J.& Park, S.J. (2021). A preference-driven smart home service for the elderly’s biophilic experience. Sensors (Basel, Switzerland), 21(1), 1-22. (PDF)
4b-2. Peters, T., & Verderber, S. (2021). Biophilic design strategies in long-term residential care environments for persons with dementia. Journal of Aging and Environment, 1–29. (PDF)
4b-3. Ryan, C. O., Browning, W. D., Clancy, J. O., Andrews, S. L., & Kallianpurkar, N. B. (2014). Biophilic design patterns: Emerging nature-based parameters for health and well-being in the built environment. International Journal of Architectural Research, 8(2), 62–76. (PDF)
4c. Horticultural Therapy
Many 18th and 19th century Almshouses in Europe featured courtyard gardens. Often, they were maintained by local volunteers or the pensioners’ families. Benefits of horticultural therapy include respite, communality with nature and its biophilia-related affordances, and socialization. Gardening is for food-consumption on-site or simply to draw people together as a seasonal (or year-round) activity. It can be part of an organized program, daily or less frequently, allowing family members to be involved. Intergenerational activities are few and far between in most eldercare facilities as it is, so it follows that friends and family should feel they are stakeholders. Gardens, including multiple small-scale gardens are effective, one per ‘house." This allows residents and others to work together towards common goals. The most typical garden type in LTC settings are raised platform flower and vegetable gardens.
For relatively ambulatory residents, standing and kneeling may still be possible, although not so the wheelchair-bound. Universally designed raised platform gardening provides all residents equal physical access and the ability to water plants from a stationary position. Platform gardening, with storage provided nearby for equipment, compliments other types of therapy. Provide seating for periodic resting and interacting with others. Provide a main flower garden as well as a decentralized network of house-based micro-gardens. These can be at grade level or housed on the roof terrace. These amenities foster intergenerationality, whereby grandchildren can partake in gardening. If the on-site horticultural therapy program is year-round, provide an all-season, enclosed winter garden/greenhouse. Provide views onto these spaces so they are not hidden away from main social activity hubs—out of sight out equals of mind. 2b; 3b; 4d; 4e; 5b; 5e; 6c; 7f

References:
4c-1. Browning, W. D., Ryan, C. O., & Clancy, J. O. (2014). 14 Patterns of Biophilic Design. New York: Terrapin Bright Green. (PDF)
4c-2. Xie, Q., & Yuan, X. (2021). Functioning and environment: Exploring outdoor activity-friendly environments for older adults with disabilities in a Chinese long-term care facility. Building Research and Information: International Journal of Research, Development and Demonstration, 50(1-2), 1–17. (PDF)
4d. Multiple Outdoor Destinations
Covid-19 brought to the forefront disconnections between the indoor and outdoor realms of most LTC facilities in the Province of Ontario. Unfortunately, opportunities had been missed in the past thirty years to incorporate the timeless attraction to nature and landscape in LTC facilities and to therapeutically draw upon this type of sensory stimulation. Interesting destination points of gardens and micro-gardens have been found to promote cognitive clarity, reduce depression, promote socialization, trigger positive mental associations from the past, and have an overall positive influence on physiologic health status, i.e. diastolic blood pressure, and physical stamina. However, it makes little sense to provide these amenities unless they are directly accessible and function as meaningful destinations. Even where such policies do exist they may be dismissed by the staff because "it is too much work" to take the resident outdoors every day when the weather is nice.
Subdivide gardens into smaller plots as multiple destination points accessed by ramps. Include a water elements such as a fountain or small waterfall, or pond safely protected by railings with pockets of seating nearby, or a gazebo and landmarks that prompt one to navigate towards these destination points—points A-B-C and so on. Orient these destinations to for maximum sunlight, with wind-blocks to buffer from extraneous noises and visual distractions. Provide shade and protection from rain so residents can be outdoors even if unable to be out in the garden that day, and opportunities to adapt as conditions change. Illuminate walking paths with lighting to accentuate multiple outdoor landmarks. Safety is of utmost priority. Wandering gardens can be designed with safe boundaries (walls, fences) where the remains in a zone with surveillance by staff, with closed-circuit monitors. Provide seating indoors overlooking these multiple destination points. 1e; 2b; 3b; 3c; 4c; 5a; 5b; 5e

References:
4d-1. Burton, E., & Sheehan, B. (2010). Care-home environments and well-being: Identifying the design features that most affect older residents. Journal of Architectural and Planning Research, 27(3), 249-250. (PDF)
4d-2. Connell, B. R., Sanford, J. A., & Lewis, D. (2007). Therapeutic effects of an outdoor activity program on nursing home residents with dementia. Journal of Housing for the Elderly, 21(3-4), 194–209. (PDF)
4d-3. Rijnaard, M.D., Van Hoof, J., Janssen, B.M., Verbeek, H., Pocornie, W., Eijkelenboom, A., Beerens, H.C., Molony, S.L., & Wouters, E.J.M. (2016). The factors influencing the sense of home in nursing homes: A systematic review from the perspective of residents. Journal of Aging Research, 6143645, 12-15. (PDF)
4e. Ecological Stewardship
Long-term care residences pollute, their toxic wastes often ending up in the local landfill. It no longer suffices for the care provider organization to hide behind public relations without at least beginning to implement ecological best practices. Opportunities exist, from retrofitting heritage buildings for use as LTC facilities (or at least as the administrative wing) to pilot projects for campus waste recycling, to sustainable land use, on-site water retention (cisterns), and micro-gardening. Why can’t LTC organizations take on a leadership role in eradicating toxic chemicals from the local water supply and food chain? In North America, the LEED-affiliated Green Guide for Healthcare began in 2003 and is a joint effort between Health Care Without Harm and the Center for Maximum Potential Building Systems. It consists of a point-based metrics system that closely parallels the mainstream LEED (Leadership Through Energy Efficient Environmental Design) certification program. These metrics are geared to specifically assess the environmental stewardship level of hospitals and allied healthcare building types.
In the U.K. the National Health Service (NHS) some years ago initiated an assessment tool called NEAT for all new construction and renovation projects and it has fostered ecologically sustainable best practices. The need exists to launch similar efforts in medically underserved communities in Canada. In the U.S., Catawba Hospital, a state-run psychiatric facility in Virginia, recently completed an extensive retrofitting of its campus, yielding significant energy savings though reduced power consumption and decreased annual facility operational costs; these savings resulted from retrofitting HVAC systems. All twenty-one buildings on the campus were retrofitted and the central chilled water plant was replaced with a new energy-efficient plant. On-demand lighting systems were installed and the overall effort has since been extended to include institution-wide stewardship to conserve the agricultural character of the natural surroundings in the Landcare Initiative project. It consists of grassland habitat conservation (to restore local quail species), and re-cultivation of warm-season grasses grown locally and judiciously harvested to help power the hospital’s heating plant infrastructure. 3c; 4h; 6d; 8b; 9a; 9h

References:
4e-1. Bentayeb, M., Norback, D., Bednarek, M., Bernard, A., Cai, G., Cerrai, S., Eleftheriou, K. K., Gratziou, C., Holst, G. J., Lavaud, F., Nasilowski, J., Sestini, P., Sarno, G., Sigsgaard, T., Wieslander, G., Zielinski, J., Viegi, G., & Annesi-Maesano, I. (2015). Indoor air quality, ventilation and respiratory health In elderly residents living In nursing homes in Europe. The European Respiratory Journal, 45(5), 1228–1238. (PDF)
4e-2. Sun, K., Specian, M., & Hong, T. (2020). Nexus of thermal resilience and energy efficiency in buildings: A case study of a nursing home. Buildings and Environment, 17(2), 1-25. (PDF)
4f. Natural and Mechanical Ventilation
The coronavirus pandemic made abundantly clear the need for proper natural and mechanical ventilation in LTC homes. The disproportionately high number of fatalities in overcrowded, improperly ventilated facilities reached crisis levels although the seeds of this disaster had been planted decades prior. For a healthcare provider organization, public or private, why was this allowed to occur? Without adequate personal distancing it was impossible to control the person-to-person transmission of Covid-19 in elderesidences in Ontario and elsewhere in North America. The problems associated with overcrowded bedrooms, personal hygiene rooms and communal areas, i.e. dayrooms and dining rooms, and the lack of meaningful options to transact with nature all contributed. These shortcomings became glaringly apparent in hundreds of LTC homes across Canada and especially in LTC homes built prior to 1990. The status quo requires thorough reappraisal, including a review of once-acceptable best practices.
Elderesidences with sealed or hard-to-open windows, inadequate HVAC systems, facilities with no air conditioning, and insufficient numbers of negative pressure rooms constitute a serious health threat. Negatively pressurized rooms combat infectious disease transmission. These rooms provide conditions where the air pressure within the room is lower than the air pressure outside the room. When the door is opened, potentially contaminated air or allied toxic particulates will not flow outside the room into adjacent non-contaminated areas. Instead, non-contaminated air will flow into the negatively pressurized room. Contaminated air is exhausted, equipped with hepafiltration and UV light fixtures to purify it before it is exhausted to the outside. Best practice design strategies include provision of an anteroom, or similar airlocked transitional zone/room. Temperature and humidity levels must be continuously monitored as the increased airflow rate can create draughts uncomfortable for the resident. There are four types of isolation rooms: Class 5, Class P, Class N, and Class Q. It is recommended these types are comparatively studied for applicability in eldercare residences. 1f; 2a; 2b; 4g; 5c; 5d; 7e

References:
4f-1. Bentayeb, M., Norback, D., Bednarek, M., Bernard, A., Cai, G., Cerrai, S., Eleftheriou, K. K., Gratziou, C., Holst, G. J., Lavaud, F., Nasilowski, J., Sestini, P., Sarno, G., Sigsgaard, T., Wieslander, G., Zielinski, J., Viegi, G., & Annesi-Maesano, I. (2015). Indoor air quality, ventilation and respiratory health In elderly residents living In nursing homes in Europe. The European Respiratory Journal, 45(5), 1228–1238. (PDF)
4f-2. Stone, P. W., Herzig, C. T. ., Pogorzelska-Maziarz, M., Carter, E., Bjarnadottir, R. I., Semeraro, P. K., Cohen, C. C., Travers, J., & Schweon, S. (2015). Understanding infection prevention and control in nursing homes: A qualitative study. Geriatric Nursing (New York), 36(4), 267–272. (PDF)
4f-3. Tartarini, F., Cooper, P., Fleming, R., & Batterham, M. (2017). Indoor air temperature and agitation of nursing home residents with dementia. American Journal of Alzheimer’s Disease and Other Dementias, 32(5), 272–281. (PDF)
4g. Theraserialization
The modernist Richard Neutra’s (born 1892-died 1970) best known works were private residences for wealthy clients in Southern California. Across a career that spanned five decades, he pioneered rational transparency vis-à-vis compositional horizontality—full height windows, natural ventilation and daylight, and therapeutic views of nature. His unbuilt hospital proposal in the 1930s similarly expressed direct contact with nature—with the majority of patient rooms provided a private balcony. The exterior environs of a LTC home provide many therapeutic opportunities of this type. The evidence-based health design literature points to the importance of strategies to maximize transparency as of therapeutic benefit. Conversely, psychologically windowless and physically windowless spaces can result in cognitive disorientation and sensory deprivation. Such conditions are of particular concern with respect to the cognitively impaired. Theraserialization is a design strategy centered on two-way transparent connective layering of exterior-to-interior space. It strategically establishes multisensory connections with nature and landscape while drawing natural light and fresh air into the building envelope.
The therapeutic serialization of architectural space can benefit the occupants of LTC homes and all healthcare building types for that matter. Theraserialization can be expressed both horizontally and vertically, and is unrestricted to only the ground plane. It is attainable at any floor level by means of terraces, setbacks, cutouts, extended eaves, recesses, light wells, atria, skylights, clerestories, and splayed axis’ whereby the envelope is sliced and pulled apart not unlike cutting through an orange. Light, view and visual axis’ legibility can foster navigational orientation. It is a useful design strategy in mid-rise 24/7 LTC facilities and especially where restricted by tight site parameters. Many of the 25 LTC case studies reported (Part I) make effective use of this strategy although there is no one best way to achieve therapeutic affordances for the building occupant. Interestingly, single-loaded corridors, connectivity with nature along exterior courtyards, and unobstructed views of nature are not new design strategies, as these features were prominent in the 32 Kirkbride insane asylums built in the US between 1854 and 1895. 1b; 2b; 3a; 3d; 4f; 5d; 5e; 7c

References:
4g-1. Barrick, A. L., Sloane, P. D., Williams, C. S., Mitchell, C. M., Connell, B. R., Wood, W., Hickman, S. E., Preisser, J. S., & Zimmerman, S. (2010). Impact of ambient bright light on agitation in dementia. International Journal of Geriatric Psychiatry, 25(10), 1013–1021. (PDF)
4g-2. Jo, H., Song, C., & Miyazaki, Y. (2019). Physiological benefits of viewing nature: a systematic review of indoor experiments. International Journal of Environmental Research and Public Health, 16(23), 4739. (PDF)
4g-3. Peters, T., & Verderber, S. (2021). Biophilic Design Strategies in Long-Term Residential Care Environments for Persons with Dementia. Journal of Aging and Environment, 1–29. (PDF)
4g-4. Verderber, Stephen. Innovations in Behavioural Health Architecture. London: Routledge, 2018.
4h. Habitat Conservation
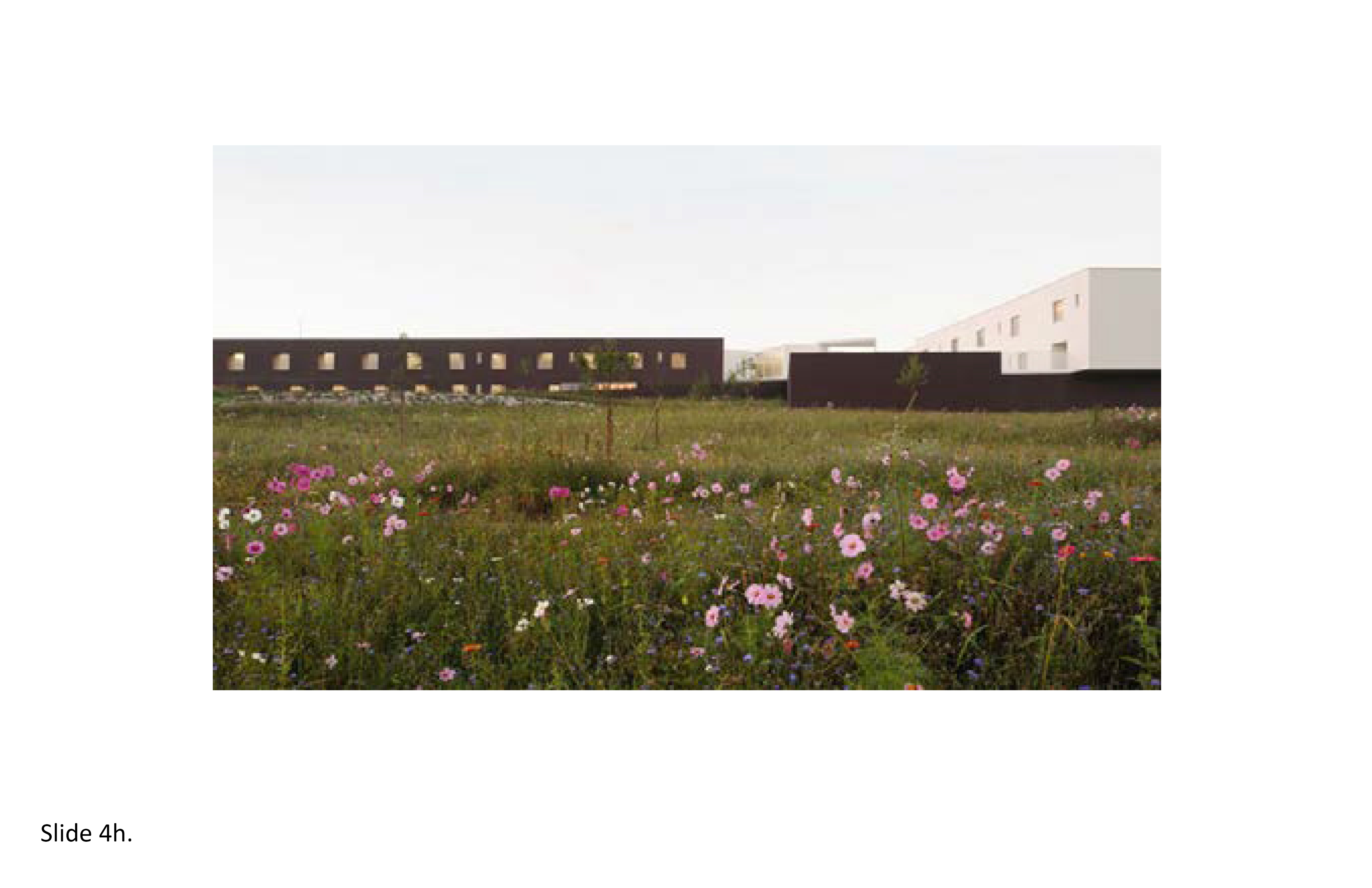
A recent report by the World Wildlife Fund (WWF) documents the dramatic decline in the world’s biospecies as they struggle to survive against an implacable and highly determined enemy in the Anthropocene: Homo Sapien. The 2016 iteration of the biennial Living Planet Report reported a 58% decline in vertebrate populations from 1972 to 2012, warning that if current trends persist unabated, the world will permanently lose innumerable wildlife species. Unbridled urbanization, the clear-cutting of rainforests (2020 set a record for destruction in the Amazon rainforest alone), massive oceanic overfishing, the list goes on—It has become imperative we rebalance habitat-species conservationism with ecologically sustainable best building practices. Too often the architectural brief will extoll the virtues of a new eldercare facility's site without mention of its adverse environmental impacts on the local ecosystems or the biodiversity ramifications. This attitudinal rebalancing must concurrently take into consideration the rapid growth in the world’s aging human populations.
How and what we build is equally important to where we build and its systemic impacts. It is recommended that multiple building footprints be comparatively examined early on in the design process in light of these concerns. Circular, bi-axial, rectangular, pointillistic, and linear footprints all warrant comparative examination for their lightness factor. Thread lightly on the site and its ecosystems. Create micro-landscapes along narrow spines to achieve transparency, lightness and sway—allowing for the preservation and further nurturing of a nearby wetland site, or wooded area. Conserve trees and when tree-cutting is unavoidable ensure that adequate replanting is part of the overall project budget. Employ cutouts and give-way irregular footprints (where feasible) such as at the Center for Cancer and Health, in Copenhagen, Denmark, by NORD Architects (2012). Many of the 25 case studies (Part I) feature footprints that protect the immediate site's ecosystem. Gone is the era of the overbuilt nursing home that exhibits little to no concern for site context or deleterious impacts on the local ecosystem. 6d; 8b; 9a; 9h; 9j
References:
4h-1. Baldwin, R. F.,Powell, R. B., & Kellert, S. R. (2011). Habitat as architecture: Integrating conservation planning and human health. Ambio, 40(3), 322–327. (PDF)
4h-2. Verderber, S., & Refuerzo, B. J. (2020). Innovations in Hospice Architecture (2nd Edition). London: Routledge.*
4h-3. Wu, J. (2019). Linking landscape, land system, and design approaches to achieve sustainability. Journal of Land Use Science, 14(2), 173–189. (PDF)
5. Circulation + Navigation
5a. Wayfinding and Orientation
Over five million in the U.S. have dementia and in Canada over 747,000 persons are living with Alzheimer’s or a related form of dementia (2022). Worldwide, at least 44 million are living with dementia—making this disease a global health crisis. With so many living much longer than in past decades, the need for 24/7 care options has never been greater and is projected to increase significantly in the coming years. In light of this, the need for memory care units in Ontario and elsewhere will only increase. An on-site memory care unit is a specialized unit that provides appropriate therapeutic support for the resident's everyday living experience. The focus on creating a positive, dignified care setting. This is achievable indoors and outdoors in physical spaces that are attuned to the resident’s functional limitations and capabilities from a press-competency perspective; a balanced physical setting in this regard will actively contribute to maximizing residents' cognitive functioning and recollection. Redundant cueing is a proven design strategy, and has been applied in LTC settings since the 1980s in the design of wayfinding directional signage systems, among other applications.
Redundant cueing consists of strategies which encode the physical setting with legible and identifiable landmarks, paths, destination points, edges, vantage points, and differentiated materials and surfaces, i.e. a floor pattern with color-coded zones and materials, recessed bedroom thresholds along corridors, and stairs clearly visible day or night through color-differentiated riser, thread, floor and wall surfaces combined with a numerical room identifier. Monotonic, poorly defined surfaces and edges lacking in legibility are to be eschewed. Single loaded corridors are effective because they afford re-orienting (cognitive re-setting) in the individual, by providing opportunities to draw daylight to the interior and views to the outdoors, along with an audio sound ("This is your room, Ms. Jones") triggered by passing through a door threshold. Together, these measures reinforce spatial orientation. Numerous multi-sensory assistive aids can help to counter memory loss and help one attain maximum degree of mastery (competency) over the immediate physical environment (and its inherent press). AI technologies will yield many design innovations to further improve spatial orientation; LTC smart-residences will anticipatorily communicate with building occupants—through prompts, messaging and non-verbal sensory cues. Circulation and other communal areas in the facility and on the grounds will then be proactive participants in anticipating potential accidents or wandering miscues before they occur by means of face recognition technology and other sensing technologies. 1b; 1e; 1f; 4d; 5b; 5c; 5d; 5e

References:
5a-1. Caspi, E. (2014). Wayfinding difficulties among elders with dementia in an assisted living residence. Dementia, 13(4), 429–450. (PDF)
5a-2. Fleming, R., & Purandare, N. (2010). Long-term care for people with dementia: Environmental design guidelines. International Psychogeriatrics, 22(7), 1084–1096. (PDF)
5a-3. Marquardt, G., & Schmieg, P. (2009). Dementia-friendly architecture: Environments that facilitate wayfinding in nursing homes. American Journal of Alzheimer’s Disease and Other Dementias, 24(4), 333–340. (PDF)
5a-4. Marquardt, G. (2011). Wayfinding for people with dementia: A review of the role of architectural design. Health Environments Research & Design Journal, 4(2), 75-90. (PDF)
5a-5. Wrublowsky, R. (2018) Design Guide for Long Term Care Homes. MMP Architects. (PDF)
5b. Controlled Wandering
The ability of a family to care for a loved one with debilitating cognitive and physical conditions is challenging and consumes enormous fiscal and emotional resources. Aside from memory loss, wandering is perhaps the most well-known behavior exhibited by aged persons with these conditions. Wandering is a common behavior in persons with Alzheimer’s and other types of dementia. Once symptoms are accurately diagnosed, an individual is thereafter deemed at risk of randomly absconding and becoming lost. Wandering behavior is distressing for families, caregivers, and dangerous for the cognitively impaired individual in search of something, or attempting to return to a place remembered from the past such as a place of work, a prior home or neighborhood, or even favorite vacation destination from long ago. Some wander because they are restless, agitated. It is important to encourage and provide support to maximize one's range of mobility and freedom of choice to enable freedom of movement in a safe, semi-independent physical setting. Wandering gardens and paths are popular in this regard, and are prominent features of the most well-known LTC residences internationally.
LTC homes with a memory care unit or Special Care Unit (SCU) for residents with cognitive disorders should feature at least one controlled wandering space—one indoors, and one outdoors. Create a secure architectural and exterior environment with locked doors, gates and provide a multi-faceted security system including visual monitoring, safe surfaces and materials, options for protection from the elements such as extended overhangs, pavilions, a sense of security at all times, a wearable tracking device, proper lighting, activities indoors and outdoors to occupy the individual’s time, opportunities for regular physical exercise, and freedom to self-choose the degree of immersion in nature and landscape. In addition, unobtrusive warning sounds should be triggered by "unsanctioned" movements, with staff alerted immediately. Avoid steps and abrupt level changes, control noise levels to avoid needless sources of agitation, and allow opportunities for socialization. Spatial autonomy may be established between a main therapeutic garden and associated wandering spaces. Indoors and outdoors, incorporate inventive multi-sensory cues to cognitively orient and reorient the individual. Eschew institutional imagery and agitating sensory cues. 4b; 4c; 4d; 5e; 7a; 7b; 7c

References:
5b-1. Algase, D. L., Beattie, E. R., Antonakos, C., Beel-Bates, C. A., & Yao, L. (2010). Wandering and the physical environment. American Journal of Alzheimer’s Disease and Other Dementias, 25(4), 340–346. (PDF)
5b-2. Chaudhury, H., Cooke, H. A., Cowie, H., & Razaghi, L. (2018). The influence of the physical environment on residents with dementia in long-term care settings: A review of the empirical literature. The Gerontologist, 58(5), 325-337. (PDF)
5b-3. Detweiler, M. B., Murphy, P. F., Myers, L. C., & Kim, K. Y. (2008). Does a wander garden influence inappropriate behaviors in dementia residents? American Journal of Alzheimer’s Disease and Other Dementias, 23(1), 31–45. (PDF)
5b-4. Detweiler, M. B., Murphy, P. F., Kim, K. Y., Myers, L. C., & Ashai, A. (2009). Scheduled medications and falls in dementia patients utilizing a wander garden. American Journal of Alzheimer’s Disease and Other Dementias, 24(4), 322–332. (PDF)
5b-5. Milke, D. L., Beck, C. H., Danes, S., & Leask, J. (2009). Behavioral mapping of residents’ activity in five residential style care centers for elderly persons diagnosed with dementia: Small differences in sites can affect behaviors. Journal of Housing for the Elderly, 23(4), 335–367. (PDF)
5c. Programmatic Decompression
In the post-WWII era, the “form follows function” dictum that drove the functionalism of the modern hospital was directly transferred to the architecture of skilled nursing institutions in North America . Nursing homes of this period expressed orthogonality, and they were bland, austere. Spartan aesthetics parsed the everyday life-care spatial and sensory needs of the "patient" (and the caregiver) into discrete functional components as if dicing up carrots. This modus operandi could be traced to the teachings of the Bauhaus (1919-1933) in Dessau, Germany. There, faculty who in time would rise to fame sowed socio-cultural imperatives to be later distilled into grocery lists of reductive, prescriptive sets of behaviors. As the offspring of the local mothership hospital, the freestanding nursing home functionally expressed what was deemed institutionally essential: minimal circulation path amenities, monochromatic spaces, and relentlessly durable, non-destructible materials—they were built as medical machines for (ware)housing the aged and infirm—"in-valid" aged persons.
LTC built environments are about far more than merely checklists of rooms and maximizing functional adjacencies. They are about expressing a multifaceted, complex program brief with the intent of establishing a home-like residential environment. The functional brief should allow room for creativity on the part of the designer to provide a variety of in-between spaces. By contrast, the application of LEAN in LTC facility planning tends to reductively systematize functional planning "best practices." Moreover, the various computer-driven space planning algorithms to optimize functional adjacencies, a practice dating from the 1960s, aimed to wring out any and all “excess” or extraneous spaces. Alternatively, the provision of various in-between spaces and zones can contribute to the resident’s quality of life because, for one, the lines of communication among staff and between staff and family increasingly occur in informal seating alcoves, hallways, dining areas and adjacent exterior spaces. This trend to provide these informal pockets of space might best be referred to as programmatic decompression—the practice of providing the interior realm a set of lungs allowing it to more fully breathe—through the acceptance of informality, randomness, and spontaneity, while injecting aspects of architectural theraserialization. This is achievable through dematerialization, spatial layering, and transparency. 1b; 1e; 1f; 4g; 5d; 6a

References:
5c-1. de Boer, B., Bozdemir, B., Jansen, J., Hermans, M., Hamers, J. P., & Verbeek, H. (2021). The Homestead: Developing a conceptual framework through co-creation for innovating long-term dementia care environments. International Journal of Environmental Research and Public Health, 18(1), 57–74. (PDF)
5c-2. De Rooij, A. H., Luijkx, K. G., Schaafsma, J., Declercq, A. G., Emmerink, P. M., & Schols, J. M. (2012). Quality of life of residents with dementia in traditional versus small-scale long-term care settings: A quasi-experimental study. International Journal of Nursing Studies, 49(8), 931–940. (PDF)
5d. Single-Loaded Circulation—Residential Zones
Single-loaded circulation spaces are an integral design strategy in theraserialization, and are antithetical to the institutionalism of the double loaded corridors of the typical nursing home. The latter are often under-illuminated and, at worst, forbidding symbols of society’s negative perceptions of hospitals as well as nursing homes. Hollywood was and remains obsessed with depicting their dehumanizing, restrictive impacts on the "patient." This was evident in the hospital scenes in Shock Corridor (1963), The Godfather (1972), One Flew Over the Cookoo’s Nest (1975), Flatliners (1999), Girl Interrupted (1999), Lost in Translation (2003), Outbreak (2004), and many other films over the decades where the double-loaded corridor played a leading role in depicting the inhumanity of institutionalization. Where do the terms double and single loaded come from? In the Industrial Age these terms likely originated as a metaphorical reference to the double and single loaded shotgun rifle. Houses in New Orleans are to this day described as single or double-loaded based on their internal circulation, meaning one could shoot a bullet through the entire house from front door out the back door without hitting a wall, as it would pass through the door thresholds of the rooms within. A double loaded shotgun house is two side-by-side long-narrow residences that share a continuous common wall.
The decoupling of the double-loaded corridor configuration in healthcare facilities began in earnest in about 2000, in single loaded psychiatric treatment centers, hospitals, hospices, and in some long-term care residences. Decoupling yielded courtyards and new types of dayrooms such as at the Corrine Dolan Alzheimer’s Center, in Ohio, which featured two triangulated wings each with a central dayroom flanked by rows of bedrooms. Later, LTC facilities were built with the center courtyard an open-air healing garden. Excellent examples were built where two bandwidths of bedrooms flanked social spaces such as at the children’s hospice in Balloch, Scotland (2005). These disengaged elements yield an informal activity zone. Some new ideas are in fact old ideas: the Kirkbride insane asylums of the late 19th century stood apart in their time, as they featured single-loaded corridors and long, narrow inpatient wings. This allowed daylight and fresh air to equally transmit into all interior circulation spaces. In this regard, the 32 Kirkbride asylums built in the U.S. are now viewed as precursors to contemporary theraserialization. While this trend may not be new, single-loaded strategies hold much promise from an infection control standpoint in LTC residential environments in the aftermath of Covid-19. 1b; 1d; 1e; 1f; 5a; 7b; 7c; 7e

References:
5d-1. Burton, E., & Sheehan, B. (2010). Care-home environments and well-being: Identifying the design features that most affect older residents. Journal of Architectural and Planning Research, 27(3), 243-246. (PDF)
5d-2. Calkins, M. P. (2009). Evidence-based long-term care design. NeuroRehabilitation, 25(3), 147-149. (PDF)
5d-3. Marquardt, G. (2011). Wayfinding for people with dementia: A review of the role of architectural design. Health Environments Research & Design Journal, 4(2), 75-90. (PDF)
5d-4. Orfield, S. (2015). Dementia environment design in seniors housing: Optimizing resident perception and cognition. Seniors Housing and Care Journal, 23(1), 58-69. (PDF)
5e. Universal Accessibility
Successful aging is predicated on the absence of disease and disability, physical and cognitive functionality, and active engagement in everyday life. Universally designed built environments provide an equal opportunity for all seniors to participate in everyday life. Universally designed spaces are attuned to the spectrum of persons with specialized needs, and allow participation in ADLs without the stigma associated with non-adaptive or “handicap-access” limitations. Universal design (UD) supports ADLs as seamlessly and unobtrusively as possible. The three main types of UD accommodations are Accessible Supports—where separate amenities, i.e. wheelchair ramps for persons with physical limitations are directly visible and usable in fulfillment of code requirements, i.e. Ontario building codes that require power door operation—push buttons, automatic sensor, on entrances to public buildings; Adaptable Supports, whereby amenities are provided that remain concealed or hidden, until needed, and physical features/equipment can be adjusted, quickly added, or removed to adapt for a specific individual: and Transgenerational Design, where the built environment is constructed from the outset to fully support individuals anticipated spectrum of physical and sensory deficits experienced in aging, i.e. power-assisted doors.
Additional UD amenities include personal hygiene-bathing devices, i.e. grab bars, bathtub/shower controls outside the fixture, lever handle faucets, non-threshold walk-in shower and bathrooms that are accessible without edges, with adjustable-height toilet and sink; Physical Ambulation: no stair climbing, no awkward door thresholds, consistent riser/tread dimensions, landings midway between levels; Food preparation: adjustable height kitchen counters, surface color contrasting, audible-tactile feedback controls, accessible ovens, microwaves with adjacent counters, and at the beyond-LTC facility scale, UD-designed retail, civic, recreational, and public transit amenities within the local community. Strive to establish a seamless continuum of UD amenities beginning with the resident’s bedroom, and extending outward to the scale of the local community. Coordinate the size, configuration and detail of the bedroom, all interior and exterior circulation paths, social activity areas, exterior landscaped spaces, parking areas, and beyond the boundaries of the immediate site outward into the neighborhood, i.e. curb cuts, adaptive audio-visual cues, redundant-cued spaces and "smart" public buildings. Architecturally, de-stigmatize the aged and the process of aging through the provision of compassionate UD amenities. 2a; 2b; 2c; 2d; 3c; 3d; 4c; 5a; 5b

References:
5e-1. Burton, E., & Sheehan, B. (2010). Care-home environments and well-being: Identifying the design features that most affect older residents. Journal of Architectural and Planning Research, 27(3), 237-256. (PDF)
5e-2. Carr, Kelly, Weir, Patricia L, & Azar, Nadia R. (2013). “Universal design: A step toward successful aging,” Journal of Aging Research, (PDF)
5e-3. Peavey, E. (2006). Linking Long-Term Care and Healthcare Facilities: Examining Typologies, Culture Change and Universal Design Features. Unpublished Independent Study, Texas A&M University. (PDF)
6. Support Amenities
6a. Maximize Caregiver/Family Supports
The modern hospital's "Geriatric Ward" made minimal provision for the patient’s family or other visitors. Overnight sleeping accommodations were nonexistent, with no kitchenettes, washrooms, or semi-private family spaces available. The modern nursing home of the late 20th century continued this legacy of un-accommodation, limiting family/visitor supports to those directly used by the patient and staff, with few exceptions. The overall lack of privacy made it difficult for family members to spend meaningful time there. In addition, nursing staff and allied caregivers were provided with few places to obtain respite. Counter-therapeutic, i.e. stressful, spatial settings have been found to be a source of LTC residents' social withdrawal, agitation, loneliness, and depression. For the caregiver, adverse outcomes can include stress, job burnout, and overall lower job performance. The absence of sufficient salutogenic (health promoting) architectural and site amenities can even contribute to elder abuse, even death, through staff inattention to the care needs of the resident.
These conditions may possibly be an indirect manifestation of excessive programmatic compression. Informal, intermediary spaces are needed where staff, family, and residents can interact away from the bedroom zone, in the semi-publicness of the dayroom and the main dining room and other places. These support spaces should straddle the line between the semi-private and semi-public realms. Alcoves, window seats, terraces, balconies, patios, and informal break-out rooms can provide cognitive affordances to allow individuals, including family and other visitors to feel they to have a place to be. Provide a kitchenette for family-visitor use, a We Work-type workspace shared by residents’ family/visitors within or close to the house, and a dedicated washroom. In Australia, family sleepover rooms are provided for the families of indigenous residents for spending multiple days on site since travel distances can be so long. This strategy is equally applicable in northern Ontario and other communities in Canada’s Far North. Provide day-only use, overnight, We Work, family and related caregiver/family supports within the residential zone and in close proximity with one or more of these spaces flanked by a residential zone on either side. 3c; 3d; 4a; 5e; 6c; 8c

References:
6a-1. Ben Natan, M. (2008). Perceptions of nurses, families, and residents in nursing homes concerning residents’ needs. International Journal of Nursing Practice, 14(3), 195–199. (PDF)
6a-2. Brown, P. B., Hudak, S. L., Horn, S. D., Cohen, L. W., Reed, D. A., & Zimmerman, S. (2016). Workforce characteristics, perceptions, stress, and satisfaction among staff in Green House and other nursing homes. Health Services Research, 51(S1), 418–432. (PDF)
6a-3. Innes, A., Kelly, F., & Dincarslan, O. (2011). Care home design for people with dementia: What do people with dementia and their family carers value? Aging & Mental Health, 15(5), 548–556. (PDF)
6a-4. Lee, S. Y., Chaudhury, H., & Hung, L. (2016). Exploring staff perceptions on the role of physical environment in dementia care setting. Dementia (London, England), 15(4), 743–755. (PDF)
6a-5. Verbeek, H., Zwakhalen, S. M., van Rossum, E., Ambergen, T., Kempen, G. I., & Hamers, J. P. (2010). Dementia care redesigned: Effects of small-scale living facilities on residents, their family caregivers, and staff. Journal of the American Medical Directors Association, 11(9), 662–670. (PDF)
6b. Artificial Intelligence
Artificial Intelligence (AI) technologies are expanding exponentially, driven by advances in machine learning. It is an area of research based in big data science and advanced predictive modeling. Future health care systems will make use of AI predictive tools in diagnosis, treatment, administration, and daily operations. These machine learning applications in health care organizations has led to widespread speculation that AI will have a large impact across the industry. Despite numerous recent medical conferences on this subject, scant adoption of AI in the healthcare industry has occurred, to date. Barriers to fuller adoption in the everyday healthcare built environment include algorithmic limitations, data access limitations, regulatory barriers, misaligned utilization incentives, and the widespread perception that AI will threaten the work of, for example, radiologists, putting them out of work due to deep learning algorithms capable of deciphering and interpreting complex image-based x-rays without humans. The perception (correctly) is that the newness of AI guarantees there are no guardrails to control its applications, nor minimum design standards with respect to the planning and design of the built environment: a classic example of technology outrunning current societal realities. 6b-1.
And yet many opportunities lie ahead to integrate AI in the LTC architectural environment, as a multi-sensory aid and universal design (UD) prosthetic modality. AI is increasingly featured in the design of Smart Houses whereby an individual's navigational movement and use of informational triggers allow the building or components thereof to speak. This redundant cueing provides assistive aid as one approaches a staircase, door threshold or other experientially divergent condition such as alerting one to a brightly daylit room after having emerged from a windowless corridor. In architectural practice, AI machine learning has great potential to critique multiple design options far more quickly and at far less cost—including surrogate modeling algorithms capable of rapid comparatively assessment, i.e., structural deformation and deformational properties of various materials and assemblies, solar radiation penetration levels, and occupants’ predictive internal movements. This is becoming known as Assistive Design Modeling, and operates in tandem with the A/E design team’s conventional design processes and tools. These machine-learned systems can be “trained” to comparatively assess a given design condition or scenario within milliseconds. 3c; 5a; 5b; 5e; 7f; 9d

References:
6b-1. Goldfarb, Ari & Teodorisis, Florenta (2022) “Why is AI adoption in health care lagging?” March 9, The Brookings Institution. (PDF)
6b-2. Tsigkari, Martha, Tarabishy, Sherif & Kosicki, Marcin (2022). “Towards artificial intelligence in architecture: How machine learning can change the way we approach design,” Foster + Partners. 29 March. (PDF)
6c. Intergenerational Connections
The premise of intergenerational housing for seniors is that their needs can be supported on a 24/7 basis with the added benefit of residing with or near younger individuals who do not require these services. The British Columbia-based company Happipad connects seniors looking for social connections and additional income with younger tenants in need of affordable housing options. Purpose-built intergenerational housing also exists in Calgary, which integrates assisted, long-term, and palliative care in a multigenerational setting. Other examples currently being built across Canada point to the benefits of living in proximity to family members, and being able to spend time with grandchildren. These ADLs function as protective, therapeutic buffers against the adverse impacts of aging, i.e. loneliness, depression, the onset of physical ailments, even death. The scarcity of affordable housing in cities and towns across Canada is currently forcing a rethinking of multigenerational housing options and how the aged can be best served in this new reality. In Ontario, until the current provincial housing crisis can be addressed, the pattern of LTC housing option scarcity is predicted to only worsen.
In Ontario, LTC homes are still thought of as a single-use/single-site proposition. Mixed-use functions that share the same site are disallowed. This stems from current restrictive funding models although examples elsewhere in the healthcare industry of intergenerational public-private funding models have been successfully built. Options exist to provide a childcare center on site, amenities for grandchildren to promote visitation such as playscapes, and in general a more normative everyday residential ambiance and aesthetic—this will draw younger persons who wish to spend time and/or live near the LTC residence. From a quality of life perspective, intergenerational connectivity is life-affirming. It is a win-win proposition with its benefits extending to all, and can result in aged residents' reduced feelings of anxiety, a greater sense of belonging, and heightened self-esteem. Place these intergenerational amenities near to and on the ground floor of the residence so useful exterior space is directly accessible. Provide shaded/screened places to sit and socialize that are safe, with a perceived sense of protection. Provide noise buffers so the sounds of children playing nearby do not needlessly disturb residents. In short, LTC facilities in Ontario and beyond need to be rethought to become models for intergenerational health and well-being. 1a; 1c; 3a; 4a; 6d; 8c
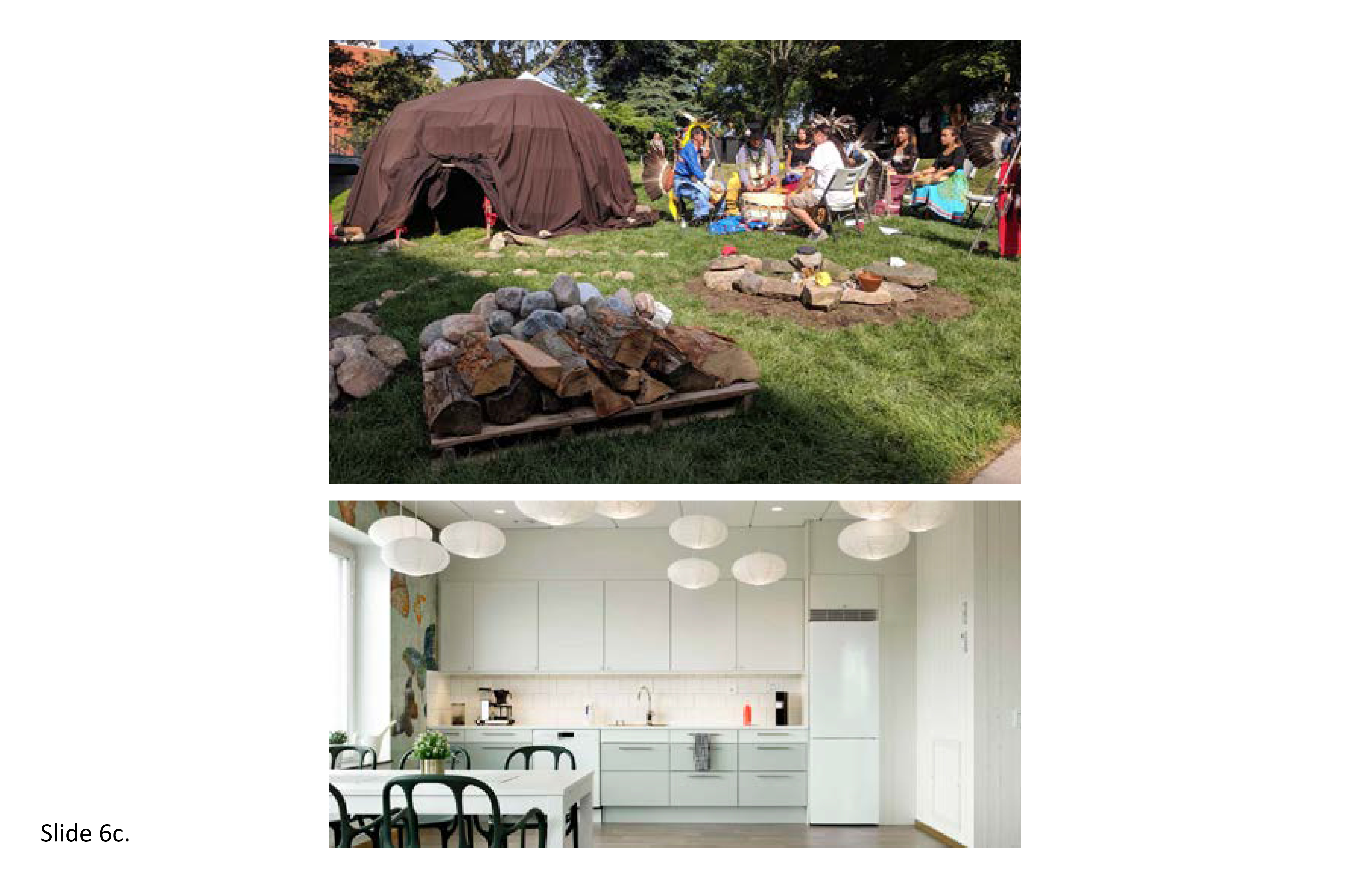
References:
6c-1. Poole, A (2019). BC Company helps seniors find young people to share a home, expenses. CBC News. *
6c-2. Suleman, Raiya & Bhatia, Faizan (2021). Intergenerational housing as a model for improving older-adult health, BCMJ, 63(4): 171-173. (PDF)
6c-3. Tan, J. Y., Tam, W. S. W., Goh, H. S., Ow, C. C., & Wu, X. V. (2021). Impact of sense of coherence, resilience and loneliness on quality of life amongst older adults in long‐term care: A correlational study using the salutogenic model. Journal of Advanced Nursing, 77(11): 4471–4489. (PDF)
6c-4. Tsai, FJ, Motamed S, & Rougemont, A. (2013) The protective effect of taking care of grandchildren on elders’ mental health? Associations between changing patterns of intergenerational exchanges and the reduction of elders’ loneliness and depression between 1993 and 2007 in Taiwan. BMC Public Health, 13(2): 567.*
6d. Aging-in-Place in the Far North
Circumpolar nations are experiencing the direct impacts of global climate change—exploitation of nonrenewable natural resources, extinction of myriad wildlife species, adverse consequences of destructive colonialist policies and practices, and growing sovereignty disputes. In a call to action, Arctic nations’ health ministers in 2016 met to sign a declaration identifying shared priorities for mutually beneficial cooperation. Collaborations are to include improving the intercultural understanding and promotion of appropriate healthcare delivery systems. Historically, and chronically, indigenous communities in Canada’s Far North have been medically underserved. This occurred because they were provided with culturally inappropriate healthcare facilities. These facilities perpetuated colonialist sensibilities and were often wholly rejected by the people for whom they were built. Such North–South cultural disconnects in Canada were allowed to persist unchecked until only recently. What is needed now are culturally-attuned elderhousing policies that allow the aged individual to remain close to one's longtime home and social supports.
Jake Paul Wolf, while a graduate student in architecture at the University of Toronto, in his thesis addressed the LTC needs of these Far North communities, where elders are currently forced to migrate (a form of forced relocation) to large hospital-like facilities geographically remote from one’s town or village. Currently, in the Northwest Territories, Northern Ontario and elsewhere across the region, elders in need of long-term residential care must relocate to a highly centralized facility. Many of these elders are Canadian residential school survivors and therefore are well-acquainted with forced relocation. Shown here is a 6-bed prototype developed for communities where the local population over age 70 is between 40 and 50 persons, i.e., Tuktoyaktuk and Aklavik; and a 12-bed prototype for communities where the elder-population ranges from 80 to 110 persons, i.e. Fort McPherson and Inuvik (all in the NWT). Each elderhouse has a “friendship centre” sponsored by the local community arts council, a sense of openness, indoor–outdoor connectivity, geothermal energy system, transitional entry vestibules, spatial informality, offsite prefab structural elements, natural daylight, window alcoves, a central firepit, garden, ritual spaces, and strong traditional connections with the land. A wood deck surrounds the residence, with nearby parking for trailers of visiting family members. Walking paths and benches afford engagement with seasonal ponds, streams, and wetlands. 1a; 1d; 1f; 2a; 2c; 2d; 3a; 3b; 3c; 4a; 4c; 4d; 4e;4h; 5b; 6a; 6c
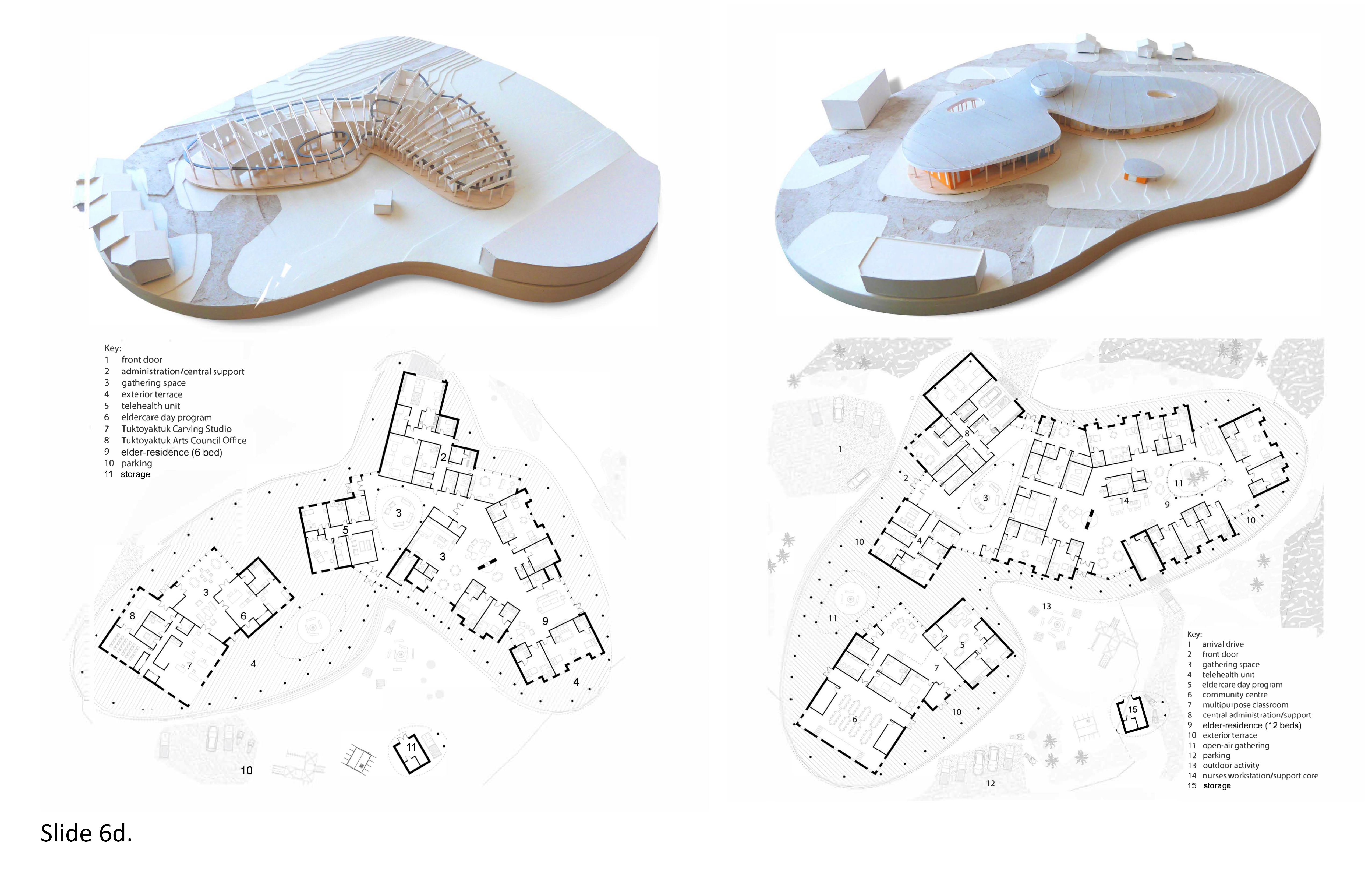
Reference:
6d-1. Verderber, S., Skouris, E., & Jake Pauls, W. (2020). Indigenous ecohumanist architecture for health in Canada’s Far North. Health Environments Research & Design Journal, 13(3), 41–56. (PDF)
7. Sensory + Environmental Support
7a. Differentiated Surfaces and Materiality
The aged experience sensory and physical deficits across the life cycle. Over time, most individuals experience one or more significant sensory deficits—eyesight impairment, physical mobility limitations, hearing loss, tactile sensitivity loss, olfactory sensory loss, and diverse mixes of sensory losses. This can result in difficulty in reading and interpreting the cues embedded in the physical environment. This is one reason why the aged are so prone to falls. In the extreme, the fear of venturing out into the world can have debilitating consequences including isolation, depression, social withdrawal, and adverse health outcomes attributed to physical inactivity. The increased probability of falls among the aged, and design interventions to mitigate their occurrence, has been the subject of evidence-based research for over thirty years. Falls are a major health problem among older adults. In the US, one in three people aged 65 and older fall at least once per year. This proportion increases to one in two for those over 80 years. Worldwide, adults aged over 70, particularly females, have a significantly higher fall-induced mortality rate than younger people. With the frequency and severity of fall-related adverse outcomes increasing with age, the most common injuries are to the head, fractures, and post-fall anxiety disorder.
Mitigation measures include the redundant cuing of architectural forms and spaces; color and material-differentiated walls and floor surfaces; smooth transitions from carpet to wood to tiled surfaces to help one achieve ambulatory spatial orientation, multi-cued directional graphics and room identification systems; stairs with color-highlighted treads and risers; adequate lighting on a 24/7 basis to adequately illuminate wall surfaces, floors, stairs and any level changes and pathways indoors and on the grounds; color-coded door thresholds; motion sensors that trigger audio cues when approaching a staircase, balcony edge, and other potentially hazardous condition. Universal design amenities include grab bars and wheelchair roll-in bathroom-shower units adjacent to the bed, and gentle-slope exterior ramps connecting, for example, an exterior garden terrace adjacent to an indoor dining room. Such amenities afford the resident opportunities to walk, interact with others and obtain exercise—thereby being pre-positioned to achieve maximum physical and sensory competency—without feeling threatened by an excessively pressing physical environment. 2a; 3a; 4d; 5a; 5d; 5e; 7b; 7c; 7e
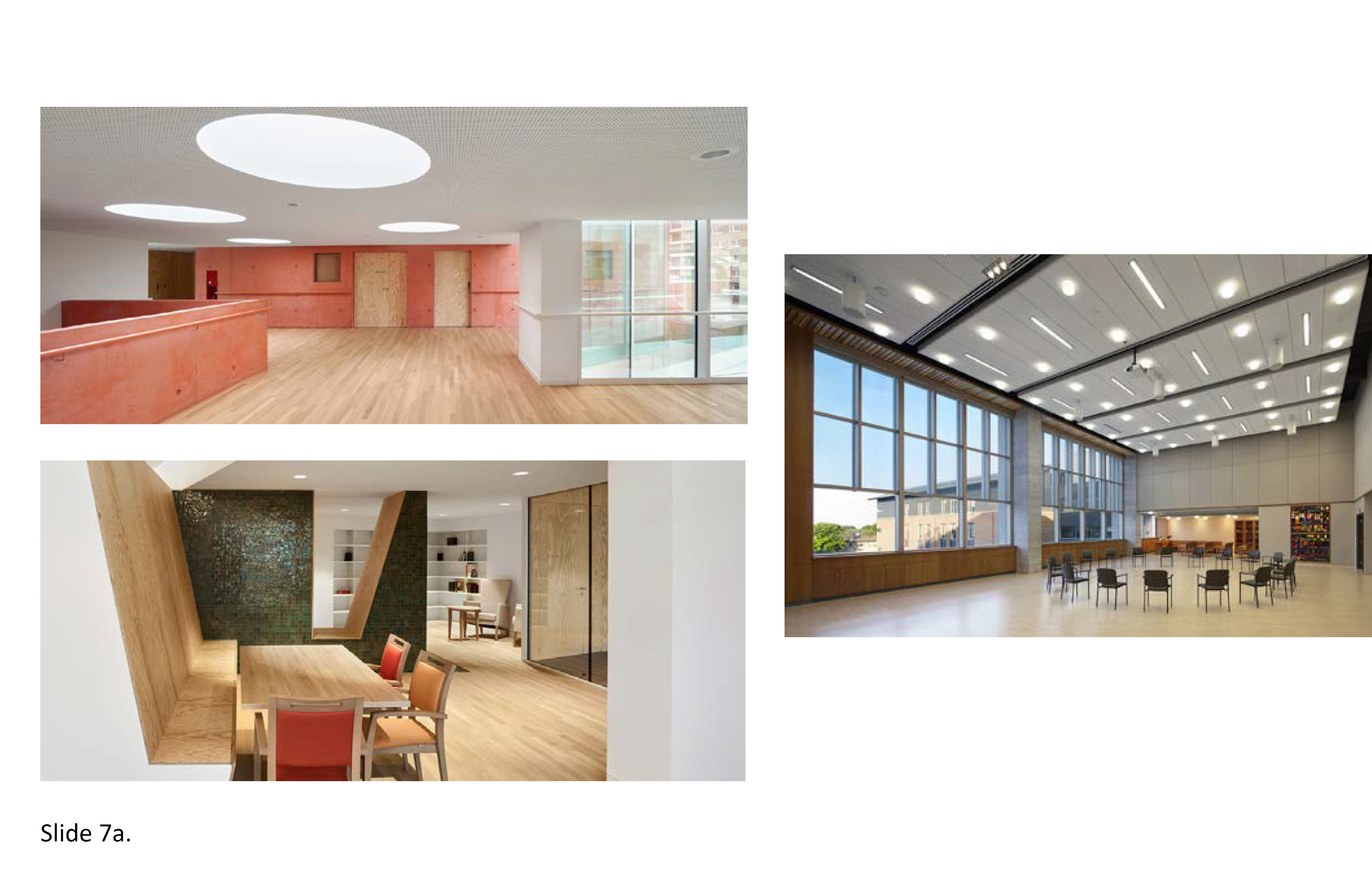
References:
7a-1. Castle, N. G., Wagner, L. M., Perera, S., Ferguson, J. C., & Handler, S. M. (2010). Assessing resident safety culture in nursing homes: Using the nursing home survey on resident safety. Journal of Patient Safety, 6(2), 59–67. (PDF)
7a-2. Jiang, Y., Xia, Q., Zhou, P., Jiang, S., Diwan, V. K., & Xu, B. (2021). Environmental hazards increase the fall risk among residents of long-term care facilities: A prospective study In Shanghai, China. Age and Ageing, 50(3), 875–881. (PDF)
7b. Eliminate Institutional Cues
The post-WWII nursing home was aesthetically drab, boring, including the thousands of repetitive International Style high-rises built where the aged lived disconnected from the neighborhoods and people they had lived among for decades. Their spartan ground floors housed most support services with lobbies featuring low ceilings, few amenities for visitors. Every floor above was entirely residential with few exceptions. Few (if any) residential units had balconies and the budget usually resulted in the exterior appearance of a hospital. Double loaded corridors underscored their institutionalism. The elimination of institutional cues requires a thorough reinvention of the type. This starts with breaking down their massive scale and height to achieve a far more humane scale with varied compositional volumes. Together with programmatic decompression, seek opportunities to design a “village” of residentially-scaled elements within a micro-campus context that promotes wayfinding, legibility and spatial comprehension. Each discrete compositional element can function as a landmark within a network of interconnected hierarchical landmarks.
Varied ceiling heights, volumes, colors, materials and imagery can inject an element of intrigue, or “lines of desire’ within the interior realm extending to adjoining exterior spaces. First impressions are important. A prospective resident and family should not feel alienated from an architecturally unwelcoming physical setting. This may seem self-evident—yet often becomes buried deep within the PPP process, governmental bureaucracy, competing financial interests, cost cutting incentives, and the seemingly ubiquitous pressure to house as many beds as possible on a single site. This is where the original design intent of eschewing institutional cues can become obliterated in a morass of competing priorities. This is avoidable, if the client and associated governmental oversight agencies from the outset establish polices that do not tie the architect’s hands before the project even begins. The overconcentration of long-term care beds on a single site, and the concept of LTC elder-residentialism need not be oppositional—with the latter yielding to the former. In Ontario, the root causes of this syndrome requires rethinking since the public pressure is great, post-Covid-19, to build as many LTC beds as possible, quickly. 1b; 2c; 3a; 4f; 5a; 5c; 7c; 7e
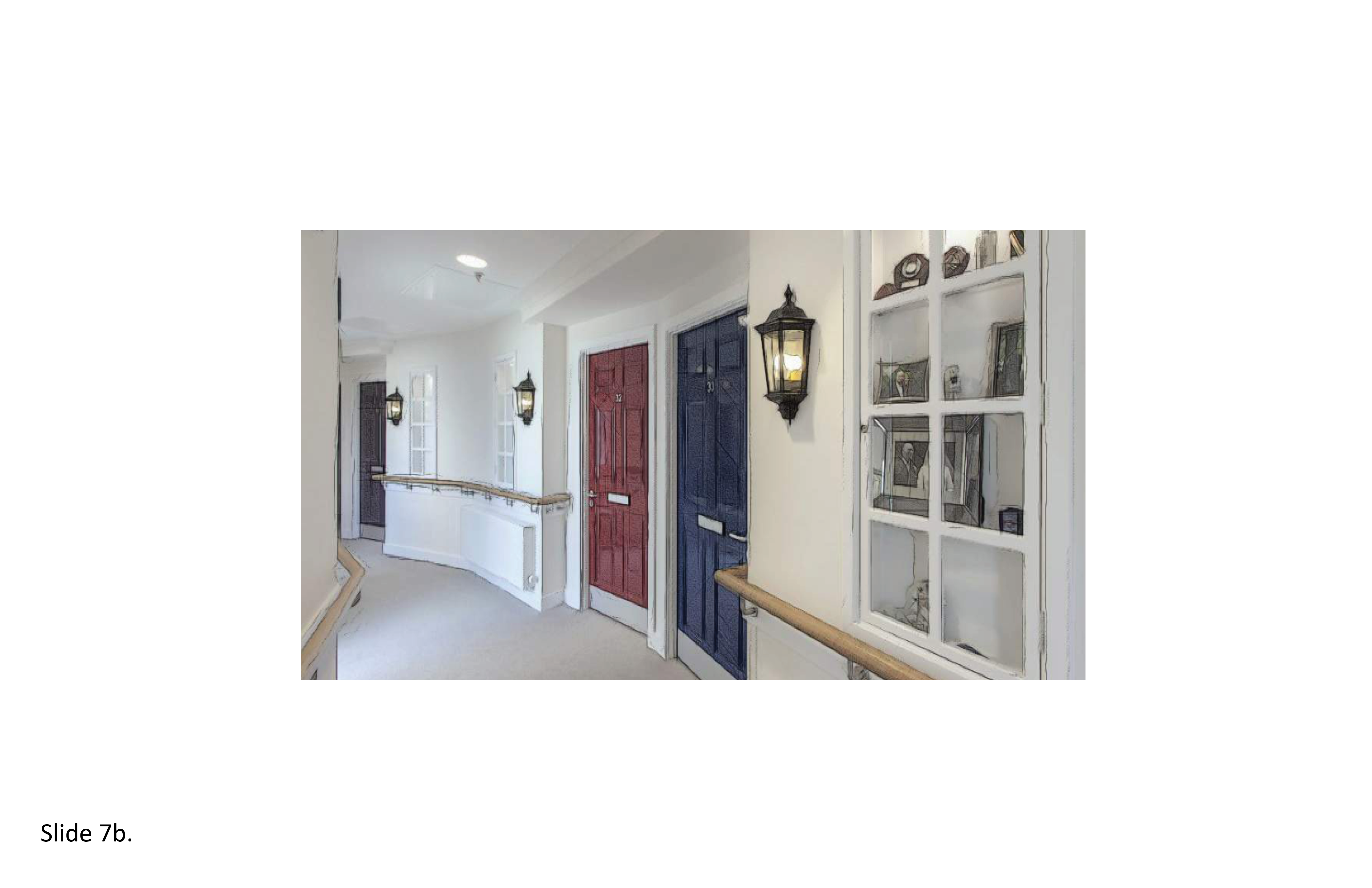
References:
7b-1. Cater, D., Tunalilar, O., White, D. L., Hasworth, S., & Winfree, J. (2021). Home is home: Exploring the meaning of home across long-term care settings. Journal of Aging and Environment, 12(3), 1–18. (PDF)
7b-2. Ferdous, F. (2021). Redesigning memory care in the COVID-19 era: Interdisciplinary spatial design interventions to minimize social isolation in older adults. Journal of Aging & Social Policy, 33(4-5), 555–569. (PDF)
7b-3. Van Steenwinkel, I., Baumers, S., & Heylighen, A. (2012). Home in later life: A framework for the architecture of home environments. Home Cultures, 9(2), 195-217. (PDF)
7c. Dynamic and Diffuse Light/Lighting
The body’s internal clock, our circadian system, regulates the timing and expression of physiological and behavioral processes, notably the sleep-wake cycle. Circadian rhythm (CR) is roughly a 24-hour rhythm controlled by the superchiasmatic nucleus (SCN) located in the hypothalamus of the brain. CRs are controlled mainly by light. The time of light exposure, duration, intensity and its spectral properties all bear upon humans’ daily patterns of living. CRs are most sensitive to short wavelength (blue) light, with a peak spectral sensitivity at around 460nm, highly prevalent during daylight hours. Many physiological changes occur with aging that affect rhythms of behaviors, temperature regulation, and hormone release, causing sleep disturbances and increased daytime napping. These outcomes are more pronounced in individuals with Alzheimer’s although persons with impaired vision and mobility are also prone to adverse CR impacts caused by under-illumination whether naturally or artificially provided. Lighting research findings indicate that bright light exposure during the day and dim light exposure at night is best suited to maintaining CRs among the aged in LTC settings. This can be problematic where few options exist to get outdoors, or if the physical setting precludes transmission of adequate natural light into the envelope, i.e. psychological windowlessness.
Structure the architectural setting to support the therapeutic application of light/lighting including ultraviolet (UV) light sources/fixtures for infection control. A lighting scheme based on cool, high light levels should be present during the day and warm, low light in support reduced circadian stimulation in the evening. A 24-hour balanced exposure to light sources has been associated with increased sleep efficiency, and lower rates of depression and agitation as measured by standardized health status indicators. Multiple types of light fixtures (incandescent, LED, florescent) and transmission apertures for natural daylight (skylights, clerestories, windows, doors) should be orchestrated to allow for users’ maximum freedom of choice so the proper balance/blend of lighting is attainable at key intervals throughout the day and evening. Exposure to artificial bright light during the night suppresses melatonin secretion, increasing sleep disturbances. Provide places indoors and outdoors for light/lighting therapy dynamics in support of prospect-refuge behaviors, balancing direct exposure with diffuse (indirect) exposure. 2a; 2b; 4g; 5a; 5d; 9a

References:
7c-1. Barrick, A. L., Sloane, P. D., Williams, C. S., Mitchell, C. M., Connell, B. R., Wood, W., Hickman, S. E., Preisser, J. S., & Zimmerman, S. (2010). Impact of ambient bright light on agitation in dementia. International Journal of Geriatric Psychiatry, 25(10), 1013–1021. (PDF)
7c-2. De Lepeleire, J., Bouwen, A., De Coninck, L., & Buntinx, F. (2007). Insufficient lighting in nursing homes. Journal of the American Medical Directors Association, 8(3), 314–317. (PDF)
7c-3. Dowling, G. A., Mastick, J., Hubbard, E. M., Luxenberg, J. S., & Burr, R. L. (2005). Effect of timed bright light treatment for rest-activity disruption in institutionalized patients with Alzheimer’s disease. International Journal of Geriatric Psychiatry, 20(8), 738–743. (PDF)
7c-4. Giggins, Om, Doyle J, Hogan K & George M (2019). “The impact of a cycled lighting intervention on nursing home residents: A pilot study,” Gerontological Geriatric Medicine, 5(1). (PDF)
7c-5. Kim, D., Chang, C., & Margrett, J. (2021). Understanding older adults’ perception and usage of indoor lighting in independent senior living. Health Environments Research & Design Journal, 14(3), 215–228. (PDF)
7c-6. Kovach, C. R., Taneli, Y., Neiman, T., Dyer, E. M., Arzaga, A. J. A., & Kelber, S. T. (2017). Evaluation of an ultraviolet room disinfection protocol to decrease nursing home microbial burden, infection and hospitalization rates. BMC Infectious Diseases, 17(1), 186–186. (PDF)
7c-7. Sloane, P. D., Williams, C. S., Mitchell, C. M., Preisser, J. S., Wood, W., Barrick, A. L., Hickman, S. E., Gill, K. S., Connell, B. R., Edinger, J., & Zimmerman, S. (2007). High-intensity environmental light in dementia: Effect on sleep and activity. Journal of the American Geriatrics Society (JAGS), 55(10), 1524–1533. (PDF)
7c-8. White, M., Ancoli-Israel, S., & Wilson, R. (2013). Senior living environments: Evidence-based lighting design strategies. Health Environments Research & Design Journal, 7(1), 60–78. (PDF)
7d. Noise Abatement
Excessive sound levels–noise—is a serious concern in all healthcare built environments. Hospitals are most notorious in this regard, followed by psychiatric and long-term care institutions. Abrupt, jarring changes in sound levels from relative quietness to a loud incident can be a source of agitation in dementia residents, and is especially problematic during evening hours. Poor acoustical conditions are frequently associated with worker burnout, absenteeism, and job dissatisfaction. In one recent empirical study, five LTC institutions were studied in Belgium before and after acoustic interventions were introduced. Sound measurements were recorded in individual bedrooms, living rooms, and corridors to identify typical levels during the day. Acoustic intra-room performance parameters (reverberation time) and inter-room performance parameters (airborne noise insulation level and impact noise insulation level) were measured and compared. It was found that noise levels in LTC homes can trigger a stress response with measurements as low as 65dB.
Also, acoustical interventions (acoustic curtains, wall and ceiling panels, ventilating grills, floating floors) were effective in reducing ambient noise. Staff caregivers rated these interventions as creating a quieter, more pleasant ambiance (7d-1). Sound is an integral dimension of communal space in long-term care that exists in midpoint tension between conditions experienced in hospital and at home. Recent research has used phenomenological methods to examine the role and function of music, and found that some sounds help to normalize the setting, drawing residents closer socially, and can help ameliorate loneliness and isolation (7d-2). Cross-cultural factors can also determine whether one’s “noise” is another person’s desirable sound. This is evidence-based justification for providing options for mitigating sound types and levels as they covary with personal privacy. Recesses and alcoves along circulation paths and at the ends of corridors for conversation or respite, with sound-absorbing materials and finishes, acoustically treated ceilings, carpeting, and double pane windows, can help lower ambient noise levels, reduce reverberation time, and heighten speech intelligibility—design features that can result in lower stress levels among staff, visitors, and residents alike. 1a; 1c; 3c; 3d; 6a; 7b
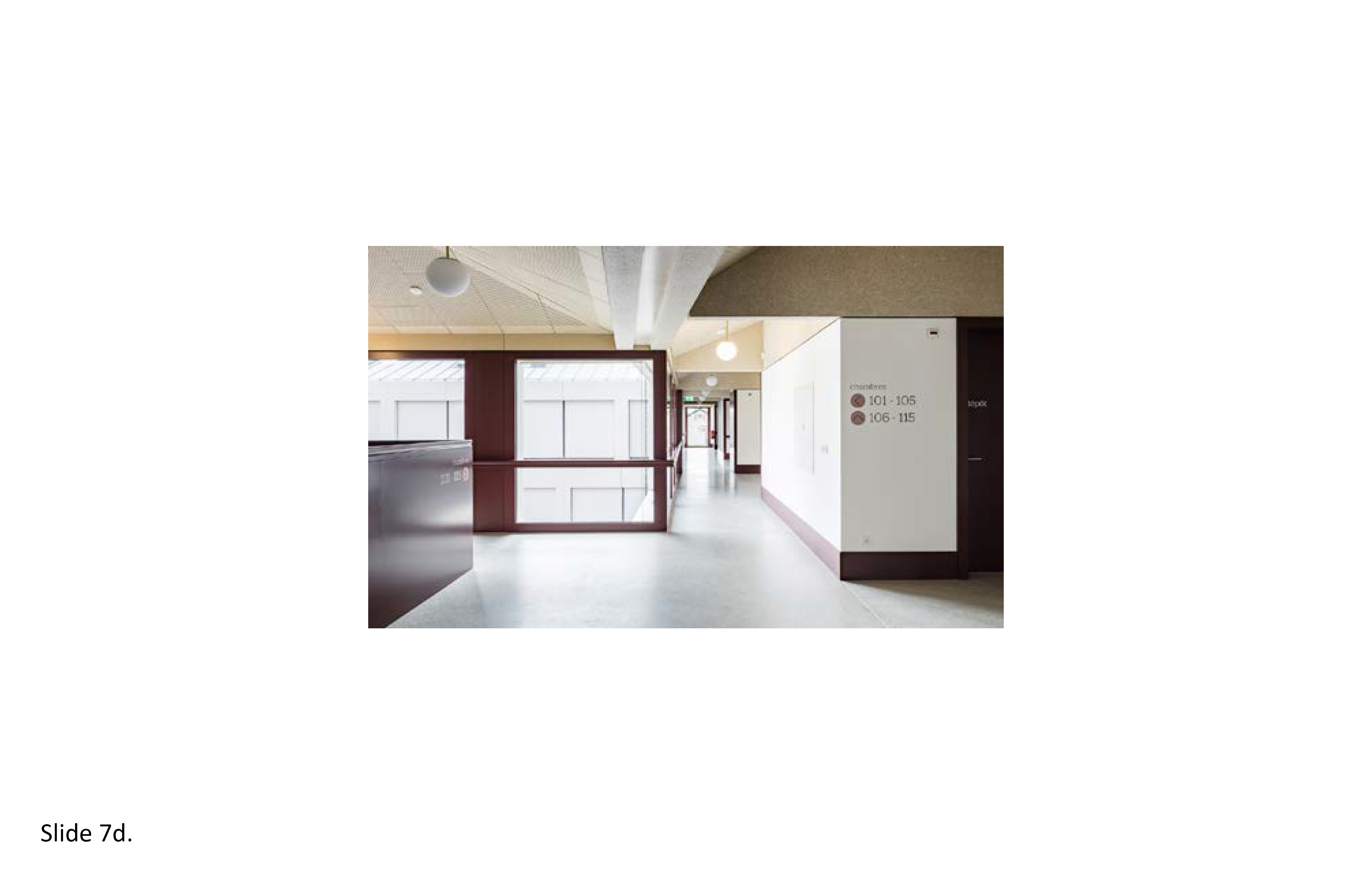
References:
7d-1. Bharathan, T., Glodan, D., Ramesh, A., Vardhini, B., Baccash, E., Kiselev, P., & Goldenberg, G. (2007). What do patterns of noise in a teaching hospital and nursing home suggest? Noise & Health, 9(35), 31–34. (PDF)
7d-2. Graham, Megan E. (2019). Long-term care as contested acoustical space: Exploring resident relationships and identities in sound. Building Acoustics, 27(1), 61-73. (PDF)
7d-3. Joosse L. L. (2011). Sound Levels in Nursing Homes. Journal of Gerontological Nursing, 37(8), 30–35.
7d-4. Joosse L. L. (2012). Do sound levels and space contribute to agitation in nursing home residents with dementia? Research in Gerontological Nursing, 5(3), 174–184. (PDF)
7d-5. Thomas, P. et al. (2020) Noise environments in nursing homes: An overview of the literature and a case study in Flanders with quantitative and qualitative methods, Applied Acoustics, 15(2), 107103. (PDF)
7e. Ambient Environment—Comfort
The thermal comfort challenge in LTC settings is to provide optimal ambient conditions for providing medical care to what can be a highly variable group of residents, and staff, for that matter. Thermal comfort standards rely on comfort models with predictive power to ascertain interior environment conditions appropriate for human occupancy. However, there are no universally accepted models for use in LTC contexts. The ASHRAE thermal comfort standard (ASHRAE 2017a) addresses environmental and human requirements, in accord with occupants’ activities and clothing type/insulation. It remains difficult to set universal standards that can be applied equally to all due to caregivers’ transient nature, age differences, and cultural differences. In general, residents prefer somewhat higher temperature levels compared to their caregivers. Further evidence-based design research is necessary in order to arrive at a universally accepted standard that can also be applied to individual healthcare types, i.e. hospitals, long-term care settings, and hospice. More broadly, on an increasingly hotter planet, excessively hot, humid conditions are beginning to result in higher mortality rates among the aged in non-air conditioned LTC homes. This must be rectified.
Due to their slower metabolic rates, older adults prefer a warmer indoor environment than younger individuals, i.e. an optimum temperature above 77 degrees F (25 degrees C) for sedentary older adults in long-term care settings. Residents with dementia are unable to communicate what is making them uncomfortable, further complicating the equation. Importantly, in light of Covid-19, negative air pressurized occupied rooms ensure toxic air will be directly removed from the building envelope. Technology-assisted window blinds and screens should be provided. Radiant surfaces are preferred, and typically cold-touch surfaces such as in bathrooms are to be sufficiently warm. Calibrate indoor humidity levels to the balanced needs of both resident and caregiver. Provide windows where feasible, opportunities to go outdoors, and push button-activated window opening and screening devices. Contributing factors: air temperature, quality, natural air movement, relative humidity, rate of air exchange (ventilation), negative pressure rooms, occupant time of exposure/intensity, overcrowding, freedom of choice, thermal insulation type, type of windows, weatherproofing, and appliances. 2a; 2b; 2c; 3c; 4c; 4f

References:
7e-1. Bentayeb, M., Norback, D., Bednarek, M., Bernard, A., Cai, G., Cerrai, S., Eleftheriou, K. K., Gratziou, C., Holst, G. J., Lavaud, F., Nasilowski, J., Sestini, P., Sarno, G., Sigsgaard, T., Wieslander, G., Zielinski, J., Viegi, G., & Annesi-Maesano, I. (2015). Indoor air quality, ventilation and respiratory health in elderly residents living In nursing homes in Europe. The European Respiratory Journal, 45(4), 1228–1238. (PDF)
7e-2. Lynch, R. M., & Goring, R. (2020). Practical steps to improve air flow in long-term care resident rooms to reduce COVID-19 infection risk. Journal of the American Medical Directors Association, 21(7), 893–894. (PDF)
7e-3. Tartarini, F., Cooper, P., Fleming, R., & Batterham, M. (2017). Indoor air temperature and agitation of nursing home residents with dementia. American Journal of Alzheimer’s Disease and Other Dementias, 32(5), 272–281. (PDF)
7e-4. Wang, Z. (2021). Use the environment to prevent and control COVID-19 in senior-living facilities: An analysis of the guidelines used in China. Health Environments Research & Design Journal, 14(1), 130–140. (PDF)
7e-5. Zhu, X., Lee, H., Sang, H., Muller, J., Yang, H., Lee, C., & Ory, M. (2022). Nursing home design and COVID-19: Implications for guidelines and regulation. Journal of the American Medical Directors Association (JAMDA), 23(2), 272-279. (PDF)
7f. Multi-sensory Stimulation
“In a multi-sensory room at Coaldale Health Centre, Herman Stroeve loops strands of color-changing fibre-optic lights about his hand like a coil of rope. The strands glow in the darkened room. As he handles them, thoroughly captivated, the long-term care resident softly reminisces about fixing a fence and mending a trough. 'We’ll see how that works,' says Stroeve, who once ran a feedlot operation. He sets down the lights, satisfied. Later, resident Evelyn Herter watches images of kittens and puppies projected onto the wall, as she snuggles a plush kitten placed in her lap by recreation therapist Jackie Scholten. 'Oh, they’re so sweet,' Herter exclaims. 'So soft!' Scholten, a recreation therapist for 18 years, had wished for a multi-sensory room for years. This past summer, her wish became a reality. Similar rooms have also been created at Cardston and Crowsnest Pass Health Centres and the Geriatric Acute Rehabilitation Unit (GARU) at Chinook Regional Hospital (all Province of Alberta).” 7f-1.
There is growing empirical support for the inclusion of a multi-sensory room (or rooms) in long-term care residential environments. These rooms provide non-pharmaceutical behavioral treatment for dementia. This treatment modality revolves around music, massage and aromatherapy, doll-animal-toy assisted therapy, and Snoezelen rooms. These measures help reduce agitation levels depending on the individual resident’s stage of dementia. Snoezelen rooms are most popular for stimulating the senses. Locate these rooms centrally but not at the heart of the most public area. Avoid potentially distracting external noise sources. An effective multi-sensory room (MSR) is a world onto itself where full immersion is attainable for varied lengths of time depending on the individual resident’s daily/weekly treatment regimen. Non-descript on the exterior, with a blank canvas interior that can become highly activated with flowing, vibrating, contrasting colors and imagery and sounds and sensations. There remains some debate on whether these rooms, where multi-sensory stimulation is therapeutically administered, are more effective than the resident's direct immersion in nature in an actual, living, outdoor therapeutic garden or in an indoor, controlled setting such as an all-season winter garden. 4a; 4c; 4d; 7a; 7b; 7c; 7e
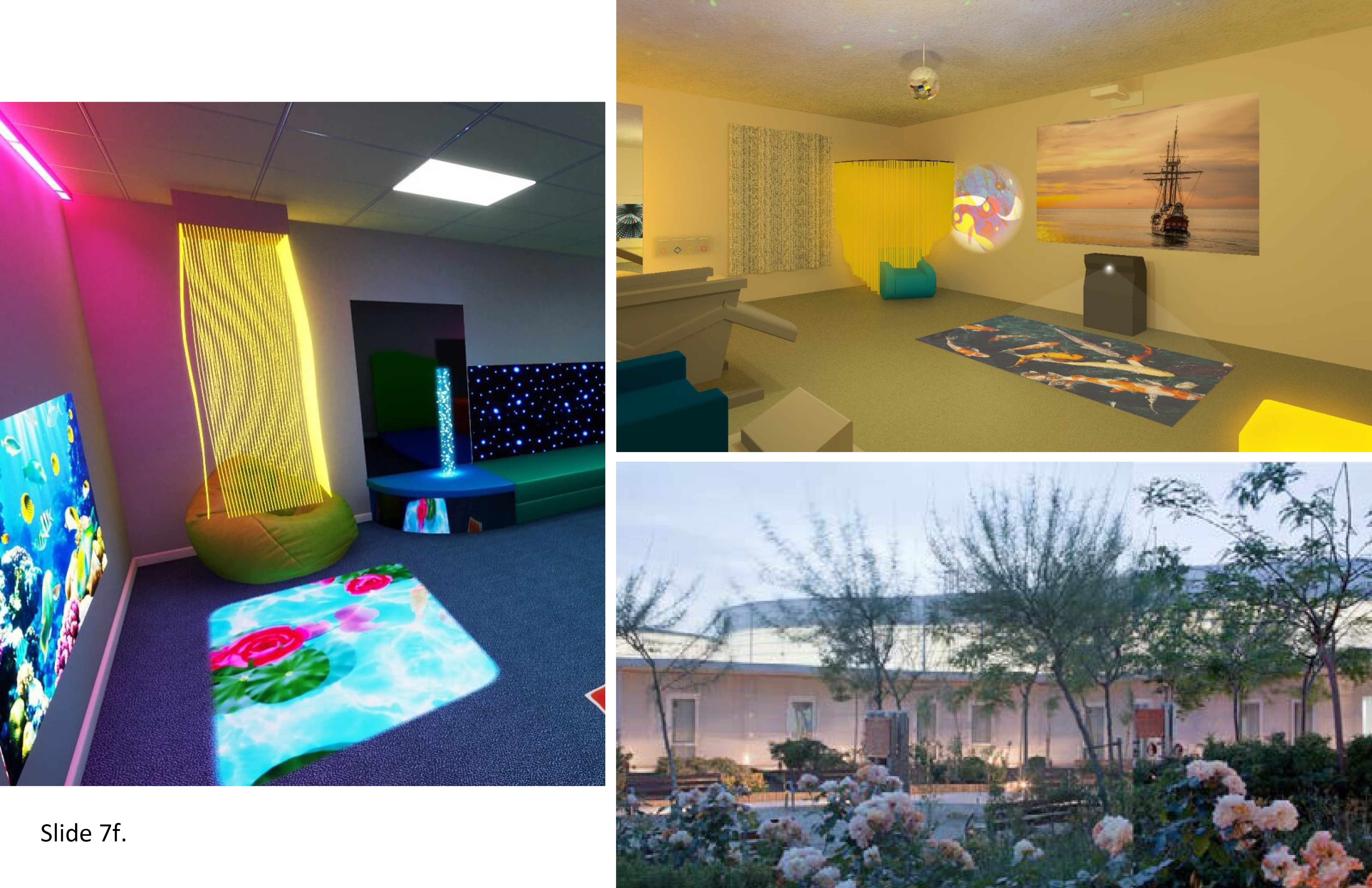
References:
7f-1. Banerjee, Srabani & Ford, Caitlyn (2018). Sensory Rooms for Patients with Dementia in Long-Term Care: Clinical and Cost-Effectiveness, and Guidelines. Ottawa: Canadian Agency for Drugs and Technologies in Health.*
7f-2. Gallant, Sherri (2017). Multisensory Stimulation Improves Quality of Life for Long-Term Care Patients. Edmonton: Alberta Health Services. https://www.albertahealthservices.ca/news/features/2017/Page14155.aspx
7f-3. Lundstedt, R., Håkansson, C., Lõhmus, M., & Wallergård, M. (2021). Designing virtual natural environments for older adults in residential care facilities. Technology and Disability, 33(4), 305–318. (PDF)
8. Offsite Prefabrication
8a. Destigmatizing Modular Prefabrication
The long-term care industry has been slow to embrace offsite prefabrication. This is due to numerous factors, including the stigma associated with prefab modularity. This type of housing has been historically associated with retirees’ trailer parks and campers, shelter types long thought of as impermanent, insubstantial, cheap, impersonal. Yet in North America this industry has moved far beyond these stereotypes, reaching a level of customization, higher quality control, advantages of labor and material cost optimization during transiting, construction, and on-site installation efficiencies. The five basic types of prefabricated structures for healthcare are—portable tent-based and pneumatic structures; vehicular nomadic (portable) units; portable or fixed-site intermodal containerized systems; portable or fixed-site flat-pack lift up and pop-up systems; and hybrid systems either fixed-site, or portable. These variants and combinations thereof provide the designer with multiple options in meeting the challenge of providing 24/7 residential care for rapidly aging societies around the globe. In short, the promise of hybrid modularity in aging societies is theoretically universal.
With regards to offsite prefab, pre-design planning, manufacturing and assembly specification of every single component part is prerequisite. First and foremost—"honor the match line”—that is, the connections between modules and all component parts. Related concerns include meticulous site prep, transiting logistics, aesthetics, production sequencing, material sourcing, HVAC and electrical systems, adaptability as occupants’ needs change, salutogenic and biophilic design amenities, and occupant safety and security. Avoid toxic materials and anything that will foster infectious disease transmissibility; do not call potentially unflattering attention onto it as a prefab. Offsite prefab modularity is a way to more rapidly provide housing for the aged in everyday residential as well as in institutional settings. Pitfalls to avoid: bland, industrial-looking systems with little aesthetic appeal; this will be viewed by occupants as undignified, depersonalizing. Recommended: Participatory design methods with key stakeholders (residents, families, staff, administrators, the local community) to test out various design options before settling on any one design concept that may inadvertently stoke the fires of local NIMBYism. 1d; 1f; 2a; 2b; 2c; 2d; 3a; 4c; 5e; 9a
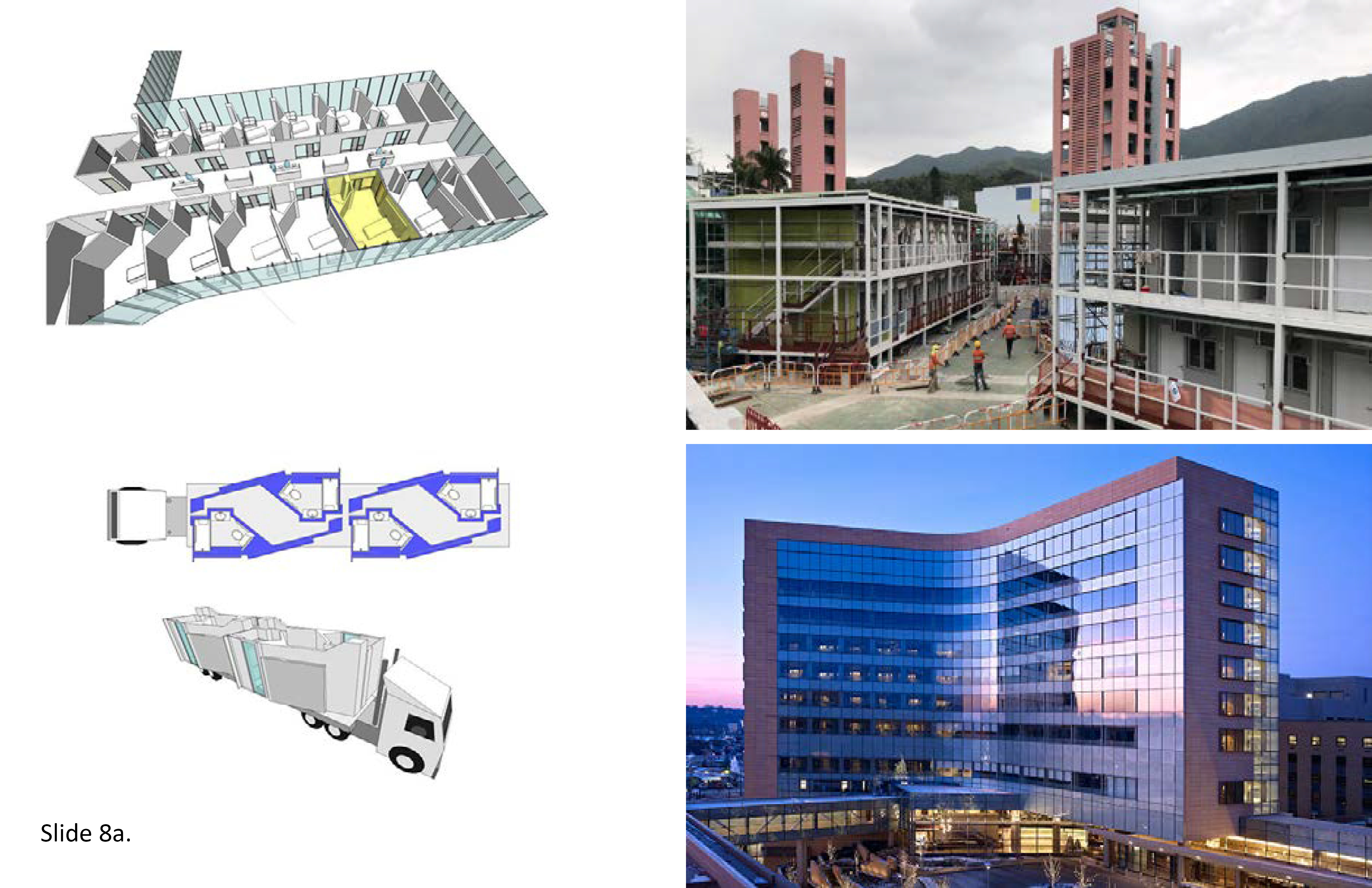
References:
8a-1. Lulo, L. D. (2009). Hybrid Prefabrication: Prototypes for green residential construction. In Clouston, P., Mann, R. K., & Schreiber, S. (eds.), Without A Hitch—New Directions in Prefabricated Architecture. Proceedings: 2008 Northeast Fall Conference of The Association of Collegiate Schools of Architecture. Amherst: MA: University of Massachusetts.*
8a-2. Peters, A. (2019). These flat pack homes can be fully assembled in less than three months. Fast Company. July 26. (PDF)
8a-3. Russo, M. (2009). Make way for modular. Multi-Housing News, 44(2), 16–17.*
8a-4. Smith, Ryan E, & Quale John D (2017). Offsite Architecture: Constructing the Future. London: Routledge.*
8a-5. Suchomel, J. L. (2018). Ready to assemble: Implementing prefabrication in health facility projects. Health Facilities Management, 31(6), 45.*
8a-6. Verderber, Stephen (2016) Innovations in Transportable Healthcare Architecture. London: Routledge.*
8b. Building in the Far North
Circumpolar nations are attracting unprecedented international attention, together with new public health challenges. This is due to the onset of climate change, the increased exploitation of nonrenewable natural resources, new sea lanes opening, the endangerment of thousands of wildlife species, and growing sovereignty disputes. In a call to action, Arctic nation health ministers in 2016 signed a declaration that identified shared priorities for mutual international cooperation. Among the agreed-upon areas of collaboration, enhancing intercultural understanding and promotion of culturally appropriate healthcare delivery systems is of high priority. In the Far North of Ontario, First Nations populations are aging at a rapid rate. The vast distances between communities in this region poses a major challenge when planning, designing, and constructing 24/7 LTC elderesidences. Standard facility procurement strategies commonplace in the southern districts of the Province often make little sense in the Far North. This is a major reason why indigenous communities in Canada’s Far North have historically been underserved, medically. The few healthcare facilities they were provided tended to perpetuate domineering colonialist sensibilities.
These culturally intrusive (even destructive) policies are now rejected by indigenous communities, ending North–South within-Province cultural disconnects that persisted for generations. Indigenous behavioral and social factors, health status, small-scale vernacular building traditions, and especially the longstanding healing role of the natural landscape are of high priority. The aged are revered in these societies and deserve to be provided with a culturally-attuned, dignified, self-empowering place to live when in need of 24/7 residential care. Second, offsite prefab modular design and construction methods make sense in places where construction is seasonally limited, roads are few and inaccessible due to permafrost melt, and building materials are scarce. However, construction labor is available and for this reason it is recommend that a 50/50 offsite-on-site building strategy be applied. This allows the local labor force to build/assemble 50% with the other 50% of all building systems and modules to be transited to the site. Cultural responsiveness: provide dozens of small-scale elder houses across the region. Participatory design strategies are essential with key stakeholders involved from the earliest planning phases. Many small-scale, in-village facilities are needed close to where the resident has lived for most if not all of one’s life—not large-scale facilities on geographically remote sites. 1a; 1b; 1c; 4e; 4h; 7b; 7c; 7e; 8a; 9f

References:
8b-1. Chatwood, S., Paulette, F., Baker, G. R., Erikson, A.M., Hansen, K. L., Erikson, H., Hiratsuka, V., Lovoie, J., Lou, W., Mauro, I., Orbinski, J., Pambrun, N., Retallack, H., & Brown, A. (2017). Indigenous values and health systems stewardship in circumpolar countries. International Journal of Environmental Research and Public Health, 14(2), 1462–1482. (PDF)
8b-2. Collinge, T. S. (2018). Indigenous perspectives on the notions of architecture. The Site Magazine, 4(6): 14–31. *
8b-3. Martin, C. (2014). Exhibition: Arctic health-care architecture. The Lancet, 384(6): 845.*
8b-4. Verderber, Stephen (2020). Indigenous ecohumanist architecture for health in Canada’s Far North,” Health Environments Research & Design Journal, 13(4): 210-224. (PDF)
8c. Accessory Dwelling Units
The increasing demand for affordable housing among Ontario’s rapidly aging population, as elsewhere, is placing heightened pressure on the Province’s real estate market. Housing unaffordability is worsening, with an increasing percentage of families unable to purchase homes at any price point. Families are being forced to move further and further from urban centers. This is referred to as drive until you qualify (for an affordable mortgage). Commuting distances are subsequently being extended, often unreasonably. This crisis requires new ways of addressing the preference for families to be able to live close enough to their loved one’s LTC home. Traditionally, from a zoning and building code perspective, the LTC home is an autonomous building type; it is programmed as an exclusive, non-mixed-use building type. Their sites are typically restricted to only the LTC home. This is social exclusionism. It is archaic. LTC home sites need to be zoned (re-zoned) for the construction more of more than only the LTC home. The Scandinavian intergenerational housing model provides innovative new ways of thinking about mixed-use/mixed-site accessory housing, or echo housing, as allowed by local codes. It is a strategy that allows for families to live in close proximity to the eldercare resident—perhaps even on the same site.
A shared-site strategy can engender community and mutual social support within an intergenerational campus setting. Explore the possibility of including, on-site, a number of accessory dwelling units—perhaps 10 to 15 homes or townhomes—for family members and visiting friends’ occupancy. These units can be owned or rented, with a few set aside for individual day rental not unlike an AirBnB. For families who reside far from the LTC elderesidence, this type of on-site accommodation can allow a family and friends to be much nearer to the resident without having to pay for a hotel or remaining geographically isolated from the resident. Explore modular offsite prefab construction options. Modular dwelling units can be located on the ground level, in a separate wing, on the roof, or otherwise physically distinct from the main facility yet on the same campus. Provide in each unit a full kitchen, minimum of two bedrooms, 2-3 baths, living space, exterior private space, with the option to dine in the LTC residence. In terms of the LTC resident’s well-being, this type of intergenerational housing holds the promise of greatly increasing the resident’s’ quality of life. 1d; 1f; 3b 6c; 8a; 9a; 9b; 9c; 9d; 9e
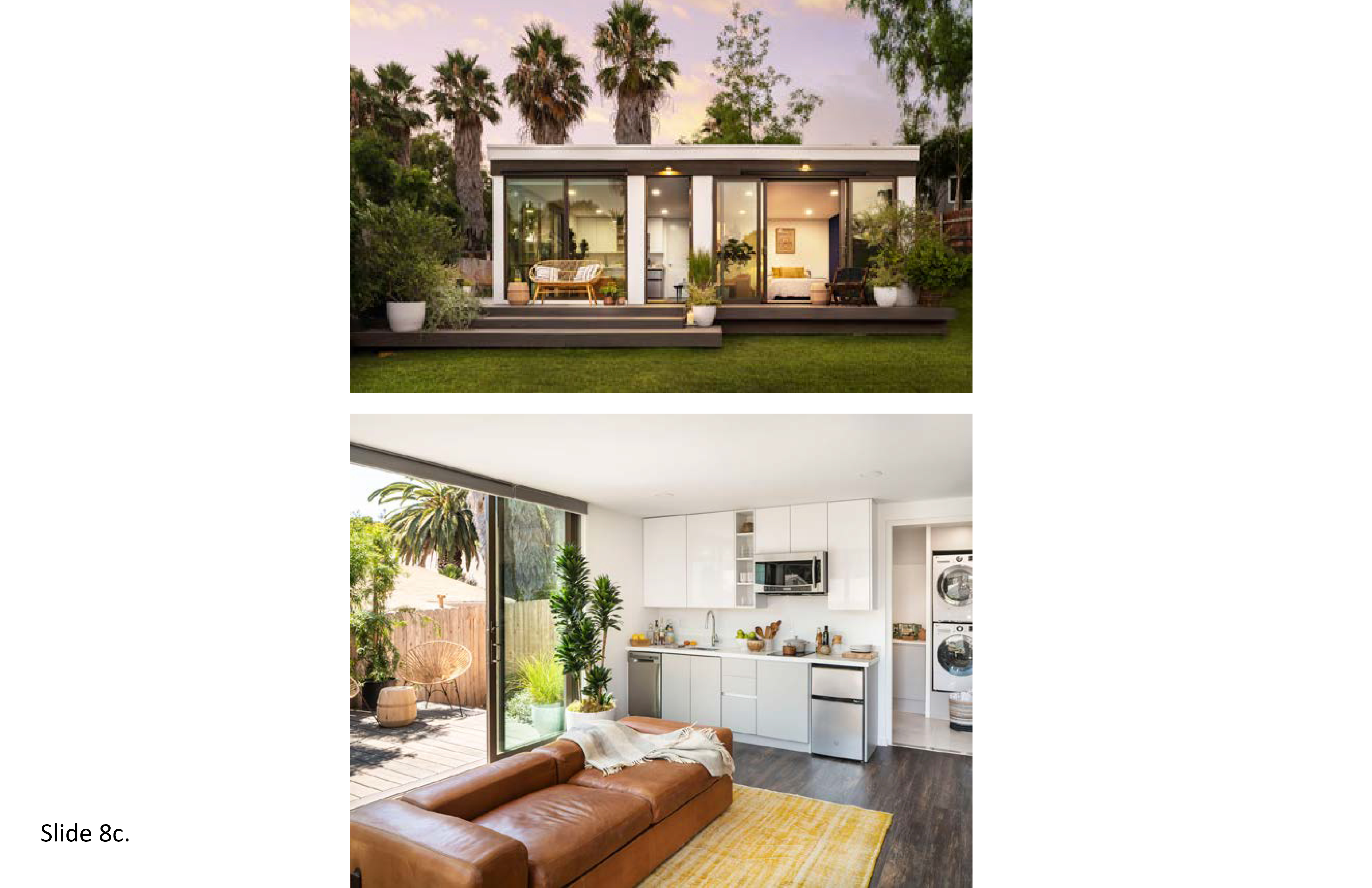
References:
8c-1. Abramsson, M., & Andersson, E. (2016). Changing Preferences with Ageing—Housing Choices and Housing Plans of Older People. Housing, Theory, and Society, 33(2), 217–241. (PDF)
8c-2. Demirkan, H. (2007). Housing for the aging population. European Review of Aging and Physical Activity, 4(1), 33-38. (PDF)
8c-3. Stevens, R., Petermans, A., Vanrie, J., & Van Cleempoel, K. (2013). Well-being from the perspective of interior architecture: Expected experience about residing in residential care centers. IASDR13, 26-30. (PDF)
9. Total Environment
9a. Site Selection and Health Promotion
The statistical correlation between unhealthy lifestyles and physical inactivity has been studied extensively. Non-communicable diseases (NCDs) are at epidemic levels among the aged in many poor and wealthy nations alike according to the World Health Organization (WHO). Sedentary lifestyles and their unhealthful consequence, especially obesity, are being documented by epidemiologists as new standards of everyday living appear and more people reside in sprawling auto-dependent urban centers. The public health community is in consensus that new strategies are needed to combat these unhealthful trends. Among the aged, comorbidities are on the rise as a function of sedentary lifestyles, i.e. eating disorders, obesity, hypertension, and depression. In North America, post-World War II suburban sprawl has fostered unhealthy lifestyles for three generations due to excessive dependency on the private automobile. Being forced to drive everywhere results in sitting still for long periods when otherwise one could have been outdoors walking or cycling between destinations.
For the LTC resident’s well-being, select a site within walking distance of a park, stores, and retail and healthcare destination points reachable on foot or via public transit such as at the Priori in Victoria, BC. For the active and semi-active aged, encourage venturing into the community for as long as possible in one’s life. The cumulative positive impacts are many. And yet a lack of sidewalks in suburbia and the long distances between destination points in everyday life often make it next to impossible to get anywhere without a car. This has had deleterious mental and physical health consequences; it remains a challenge for transportation planners to get people out of their cars. Building new eldercare residential campuses far from urban cores only exacerbate this syndrome—Instead, providing geographically compact connection points between LTC homes and off-site local amenities. For the benefit of families with a loved one residing in a 24/7 eldercare residence, seek out buildable sites near health-promoting transit infrastructure—this can result in increased visitations by family members and others. 1a; 4e; 4h; 5e; 6d; 9b; 9d; 9e; 9g

References:
9a-1. Alley, D., Liebig, P., Pynoos, J., Banerjee, T., & Choi, I.H. (2007). Creating elder-friendly communities: Preparations for an aging society. Journal of Gerontological Social Work, 49(1-2), 1-18. (PDF)
9a-2. Aung, M., Koyanagi, Y., Ueno, S., Tiraphat, S., & Yuasa, M. (2021) A contemporary insight into an age-friendly environment contributing to the social network, active aging and quality of life of community resident seniors in Japan, Journal of Aging and Environment, 35(2), 145-160. (PDF)
9a-3. Wu, J. (2019). Linking landscape, land system and design approaches to achieve sustainability. Journal of Land Use Science, 14(2), 173–189. (PDF)
9b. Engage the Local Community
As of January 2022, 79,000 qualifying individuals in the Province of Ontario were on waiting lists for home-based eldercare services, and nearly 38,000 qualifying individuals were on waiting lists for LTC homes. This is where the problem usually begins—a community’s worsening shortage of seniors’ services due to a lack of planning. The architectural community in Ontario, as represented by the Ontario Association of Architects—has focused on improving the quality of long-term care architecture. Through its committee structure it has engaged with elected officials and others at the Provincial level long before the start of the Covid-19 pandemic. The need for more LTC beds in the Province had repeatedly been documented in the years prior to the pandemic. The architectural community is ready to act but it needs for the government to streamline the facility procurement process. The status quo is unacceptable.
Healthcare organizations and their A/E teams often do not participate to the extent they can to engage the community where they seek to build a new LTC home. Yet this should be the cornerstone of a Province-wide effort to fill the unmet need, especially in underserved parts of Ontario. Strategies for community engagement have been proven to work at the local level. One way to engender the trust and buy-in from the local community, from a leadership perspective, is through genuine efforts to simply listen and then respond to what one has learned through the community consultation process. Listen to various local stakeholder constituencies and to what they care about most, then translate this information into evidence-based, responsive (responsible) built form. Work to create an atmosphere of mutual respect, acknowledging that the status quo might be less than unsatisfactory. It is well-known that basic funding for services for home-based, and institution-based LTC needs to be increased, with basic protections for the human rights of the aged and their families strengthened—but it all begins with trust. 4e; 4h; 6c; 9a; 9d; 9i; 9j

Reference:
9b-1. Buffel, T., Phillipson, C., & Scharf, T. (2012). Ageing in urban environments: Developing ‘age-friendly ‘cities. Critical Social Policy, 32(4), 597-617. (PDF)
9c. Resident and Caregiver Safety
As Covid-19 so painfully demonstrated, the built environment is a primary host for the transmission of airborne infectious disease. Infection rates are but one outcome metric of a LTC home’s overall safety. According to the Centers for Disease Control and Prevention (CDC) each year an estimated 648,000 people in the U.S. develop hospital-acquired infections and nearly 75,000 of these victims die. Many such illnesses and deaths are directly traceable to the use of pathogenic antibiotics, the very drugs whose purpose is to fight and eradicate infection. Long-term care residents can be less cooperative in terms of maintaining proper personal hygiene, adhering to prescribed medication protocols, and other related sickness and disease prevention measures. The aged resident may also have a history of comorbidity, chronic infection due to a history of substance addiction or a mental disorder, human immunodeficiency virus (HIV) infection, hepatitis B or C, or tuberculosis. These immunocompromising conditions can pose a heightened risk to other residents’ health, and that of the staff.
Aged individuals with dementia and related cognitive disorders deserve a dignified care setting neither threatening nor disempowering. Apart from infection control, recent advancements in security/surveillance technologies make it possible to establish layered, overlapping zones of security beginning at the campus perimeter, to the heart of the facility, as concentric rings culminating in the residential unit. Provide secure buffer zones at the outer edge, in parking areas, up to the main entry, into the internal semi-private and private zones. These technologies should be unobtrusive—infrared imagery, lasers, CCTV, and card reader sensors at access points. Balance advanced security measures with the care philosophy—distinguishing between static security (fixed, static devices) and dynamic/fluid security. The more invisible the security intervention, the better, to help ensure the security system is seamlessly integrated into the architectural and landscape environment. This will avoid costly retrofitting later. Emphasize a residential ambiance and appearance. 2a; 2d; 5b; 5e; 6a; 9g; 9i
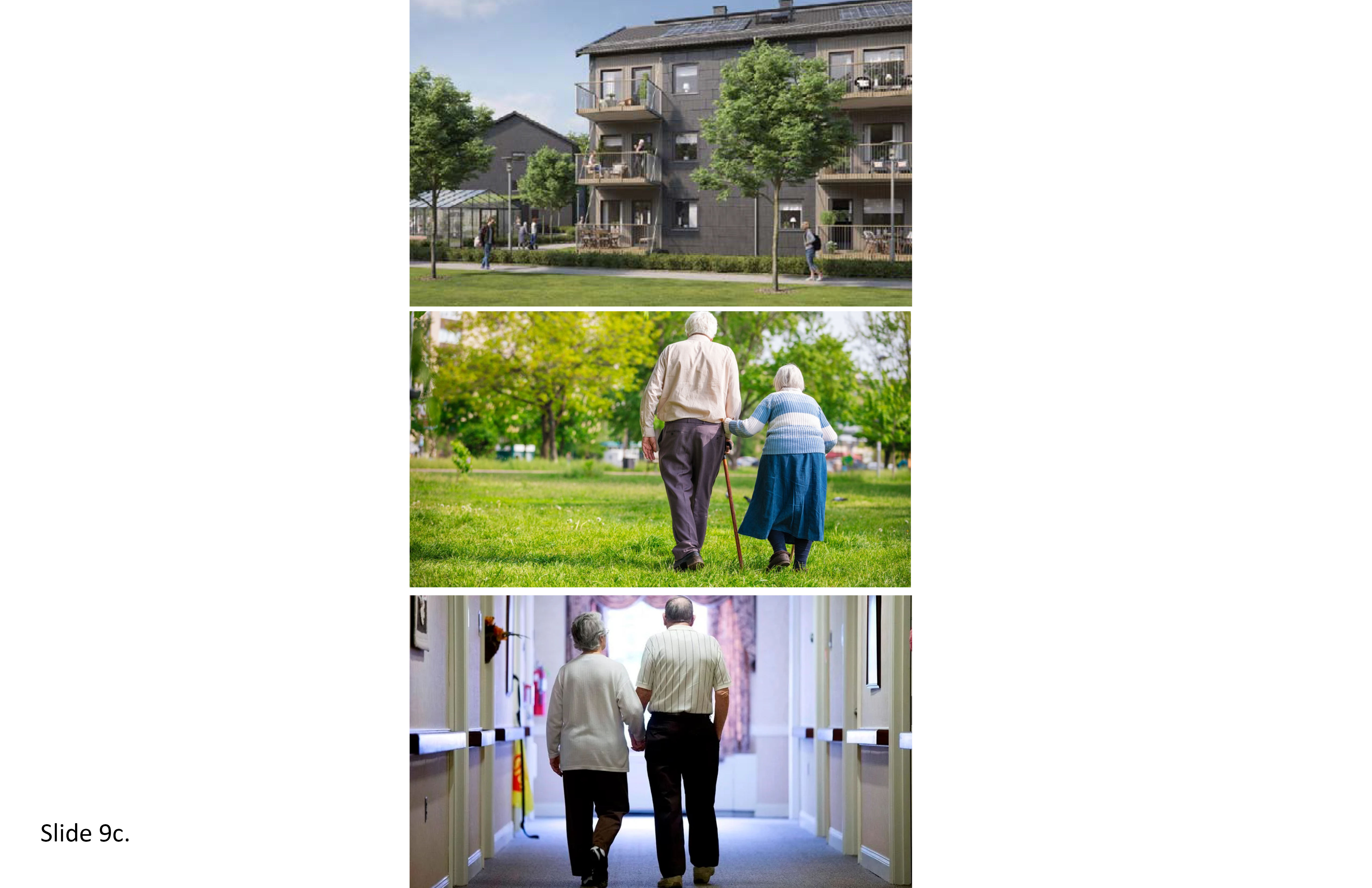
References:
9c-1. Brown, K. A., Jones, A., Daneman, N., Chan, A. K., Schwartz, K. L., Garber, G. E., Costa, A. P., & Stall, N. M. (2021). Association between nursing home crowding and COVID-19 infection and mortality in Ontario, Canada. JAMA Internal Medicine, 181(2), 229–236. (PDF)
9c-2. Castle, N. G., Wagner, L. M., Perera, S., Ferguson, J. C., & Handler, S. M. (2010). Assessing resident safety culture in nursing homes: Using the nursing home survey on resident safety. Journal of Patient Safety, 6(2), 59–67. (PDF)
9c-3. Chu, C. H., Donato‐Woodger, S., & Dainton, C. J. (2020). Competing crises: COVID‐19 countermeasures and social isolation among older adults in long‐term care. Journal of Advanced Nursing, 76(10), 2456–2459. (PDF)
9c-4. Innes, A., Kelly, F., & Dincarslan, O. (2011). Care home design for people with dementia: What do people with dementia and their family carers value? Aging & Mental Health, 15(5), 548–556. (PDF)
9d. Constituency Empowerment
In most Western societies, the aged lack sufficient voice. Often, neither they nor their families are involved sufficiently in decision-making on the best available care options. A high percentage of seniors are chronically exposed to social exclusion, shunning, bullying and various forms of discrimination. Self-empowerment begins with confronting this persistent problem. It entails reclaiming one’s sense of worth, personal competencies, sense of control, in recognizing and releasing the hidden power harnessed in positive, mutually supportive, life-affirming interpersonal relationships. It not a destination per se, but a journey. It is about the LTC Bill of Rights in Ontario, combating stigma, access to information and resources, being included in decision-making, and compassion. It is about home-based elder-health services, community-based health clinics, and their governing structures. It is about being consulted in a meaningful way whenever the service provider is contemplating a capital improvement initiative, whether a renovation of an existing facility or when planning the replacement of a LTC home.
It is being allowed to engage in the public discourse, with meetings scheduled at convenient times, and to genuinely be listened to—versus hidden agendas or being accorded superficial ‘lip service’ just so the decision-making parties can say that they “heard people out.” It is about being consulted on the location, size, and design of a proposed new LTC facility and its grounds, transportation linkages, master plan phased growth options over time, and its ecological impacts. In the U.K., the Bradford City Clinical Commissioning Group recently began an initiative it calls Grass Roots, drawing local stakeholders together in consultation in the review of specific healthcare projects, new proposed therapy and counseling resources, and in the establishment of effective communication vehicles for soliciting local mental health advocacy groups’ input. More than 1,949 online posts related to patient and family feedback were received from 3,987 individuals, with 209 of these coming directly from former mental health patients and their families. This can happen in Ontario, with the professional architectural community taking on a lead advocacy role. 2c; 3c; 4a; 6a; 6c; 9b; 9c; 9i
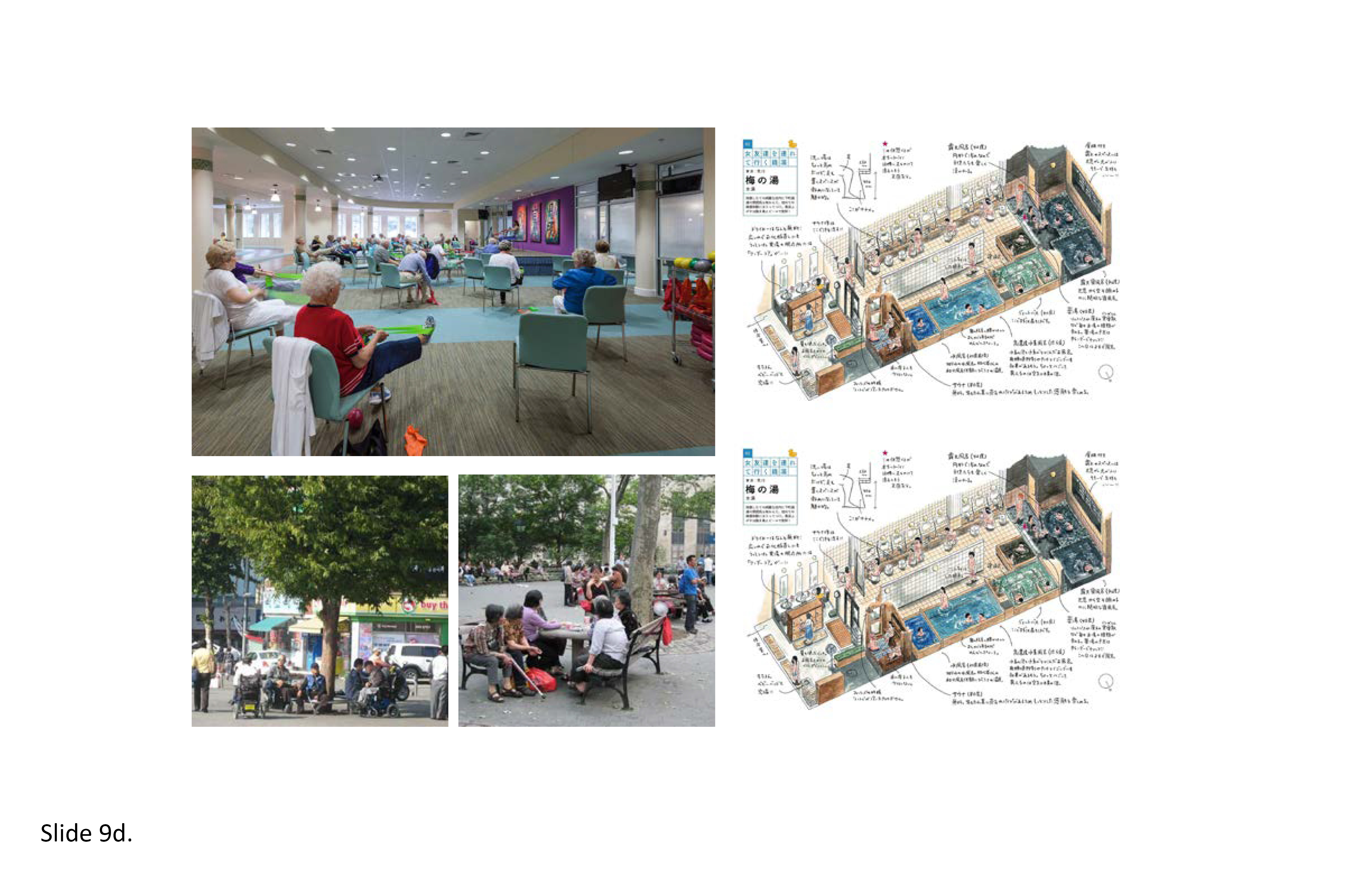
References:
9d-1. Canadian Association for Long Term Care. (2017). Caring for Canada’s Seniors: Recommendations for Meeting the Needs of an Aging Population. (PDF)
9d-2. Söderberg, M., Ståhl, A., & Emilsson, U. M. (2012). Family members' strategies when their elderly relatives consider relocation to a residential home—Adapting, representing and avoiding. Journal of Aging Studies, 26(4), 495-503. (PDF)
9d-3. Steele, L., Carr, R., Swaffer, K., Phillipson, L., & Fleming, R. (2020). Human rights and the confinement of people living with dementia in care homes. Health and Human Rights, 22(1), 7-19. (PDF)
9d-4. Wang, C., & Kuo, N. (2006). Zeitgeists and development trends in long-term care facility design. The Journal of Nursing Research, 14(2), 123–132. (PDF)
9e. Net Zero Strategies
Life-Cycle Assessment (LCA), eco-balancing, and cradle-to-grave building performance metrics take the long view in assessing facility operational performance. The aim is to maximize regenerative sustainability through the evaluation of ways to reduce the environmental impact of a building. Positive-net gains are accruable in the form of givebacks. This begins at the earliest stages of a capital improvement process and it involves key stakeholders. The facility’s occupancy lifespan is first defined, be it 20, 30 years or longer. Assessment includes all building materials and assemblies, structural and environmental control systems, the type of construction, maintenance and upkeep determinants, all relevant growth and retrofit options likely to play out over the pre-set lifespan timeframe, human health status and occupant satisfaction and performance metrics, biohazardous and solid waste disposal factors, and anticipated campus-facility resilience in the face of external threats. This process is dependent on both internal/external data streams but remains hampered by the one-off (customized, largely on site-built) nature of the major share of healthcare construction projects today.
Numerous software tools allow the owner to anticipate various outcome scenarios, and when they will likely occur relative to multiple site planning and building design options. These include climate change variables such as the effects of atmospheric acidification, eutrophication, fossil fuel depletion, smog formation, ozone depletion, ecological toxicity, and on-site water retention and recycling. Multiple data input/outputs are analyzed and assessed for their predicted performance. Environmental programs for practical application include ISO14000—the most generally applicable and flexible program—developed by the International Standards Organization (ISO), the British Research Establishment Environmental Assessment Methodology (BREEAM), launched in 1990, BREEAM Canada, and BREEAM/Green Leaf. In 1996, this program was introduced to Canada and is now known as the CSA Plus 1132 Standard. The Green Building Challenge (USGBC) is an international building assessment tool in many ways equivalent to the well-known LEED program in North America. In Australia, the National Australian Building Environmental Rating System Project (NABERS) is gaining momentum. Recently, embodied energy has come to the fore—the sum of the energy required to extract the raw materials and then produce, transport, and assemble the building on-site. 4e; 4h; 8a; 8b; 9g; 9h; 9j

References:
9e-1. Brownell, Elaine (2016) Understanding embodied energy in design, Architect, 29 April.*
9e-2. Guenther, R & Vittori, G. (2013). Sustainable Healthcare Architecture. Second Edition. New York: Wiley. *
9e-3. Halloway, K. (2019). The building of a net zero hospital. Health Facilities. 26 June. *
9e-4. U.S. Environmental Protection Agency (2010) Defining Life Cycle Assessment, Washington, D.C. *
9f. Evidence-based Research for Design
The CEO of a long-term care organization occupies a vital leadership role. Administrative policies must translate into strong organizational performance including the day-to-day performance of the facility. Zimring, et al. (2008) put forth an evidence-based facility procurement process premised on according careful attention to strategic business planning, facility and campus master planning, transitional planning to ensure smooth operations in relocating from an existing to a new facility, programming, design and construction, and with the provision of continued oversight throughout the commissioning and post occupancy retrofitting phases across time. This process is ideally driven by placing the primary emphasis on the well-being and aspirations of those who inhabitant the LTC home on a daily basis, including residents’ family member stakeholders. In the U.S., the Institute of Medicine report “To Err is Human” (1999) launched the patient-staff safety movement in hospitals and in allied healthcare built environments. Perhaps the recent report released by the National Academies of Science, Engineering and Medicine (2022) on LTC will do the same.
In both reports, evidence-based knowledge is viewed as foundational. The patient safety movement in acute care hospitals combats the high incidence of hospital-acquired medical errors and adverse events. Accordingly, it now behooves LTC provider organizations to accept and adopt evidence-based knowledge in the shaping of health policies that will improve the everyday inhabitability of seniors’ homes. Top-down corporate initiatives will likely fail if initiated mainly for marketing, PR, or capital fundraising purposes: opaqueness and insincerity often backfire, accomplishing little in the long run. Work to help the client foster hybrid top-down/bottom-up evidence-based facility planning and design strategies grounded in measurable outcome metrics. Make these evidence-based metrics accessible to key external stakeholder advocacy groups in the community. Translate the current evidence-based knowledge available on LTC built environments into built form. Follow up the occupancy phase of the new or renovated facility and its immediate environs with an evidence-driven building and site performance (POE) assessment. 2a; 2c; 5e; 6a; 9a; 9b; 9c; 9i; 9j

References:
9f-1. National Academies of Sciences, Engineering, and Medicine (2022). The National Imperative to Improve Nursing Home Quality: Honoring Our Commitment to Residents, Families, and Staff. Washington, DC: The National Academies Press, (PDF)
9f-2. Cutler, LJ, and Kane, RA, Post occupancy evaluation of a transformed nursing home: The first four Green House settings,” Journal of Housing for the Elderly, 23(4), 304-334. (PDF)
9f-3. Orfield, S. J. (2013). Aging research, design education, and the perceptual limits in seniors housing design: Development of a research-based design model for better aging environments. Seniors Housing & Care Journal, 21(1), 136-144. (PDF)
9f-4. Preiser, Wolfgang F.E., Andrea Hardy and Ulrich Schramm (eds.) Building Performance Evaluation: From Delivery Process to Life Cycle Phases. New York: Springer, 2018.*
9f-5. Zimmerman, S., Bowers, B. J., Cohen, L. W., Grabowski, D. C., Horn, S. D., & Kemper, P. (2016). New evidence on the Green House Model of nursing home care: Synthesis of findings and implications for policy, practice, and research. Health Services Research, 51(S1), 475–496. (PDF)
9f-6. Zimring, C., Godfried, L. Augenbroe, E., Malone, B., & Sadler, B.L. (2008) Implementing healthcare excellence: The vital role of the CEO in evidence-based design, Health Environments Research & Design Journal, 1(3): 7-21.*
9g. Disaster Preparedness and Resiliency
Every healthcare organization should have an emergency preparedness plan. A strategic plan of this type will be of benefit in anticipating climate change impacts, i.e. rising sea levels, intense rainstorms, hurricanes and typhoons, periods of drought and associated water shortages, and related events likely to impact population migration patterns and the quality of life in the coming decades. In the case of St. Rita’s nursing home in St. Bernard Parish in suburban New Orleans, the floodwaters from Hurricane Katrina in 2005 filled this one-level facility nearly to the ceiling within twenty minutes. The owners were later put on trial on 35 counts of negligent homicide and 24 counts of cruelty to the elderly and infirm patients who drowned in their beds and wheelchairs. The owners maintained that keeping these frail patients in place was safer than subjecting them to the trauma of forced evacuation. Eight long years later, the owners of the nursing home were eventually acquitted of guilt in their deaths, yet this tragedy serves as a cautionary tale for mental health and addiction disorder service providers everywhere.
While this is an extreme example, the fact remains that every long-term care organization should have an emergency action plan in the event staff and patients must be evacuated offsite, or to safe quarters elsewhere on-site. The adverse consequences of poor disaster preparedness can be felt for decades after the disaster event itself. Install extra security measures in anticipation of acts of elder-abuse when a facility is in pre-disaster lockdown or in the process of being evacuated. In high-risk zones it is advisable to hold preparatory evacuation drills frequently to pretest the emergency preparedness plan. Rapid response is the difference between life and death. Include such plans from the outset of the LTC capital improvement project, with built-in resiliency measures as part of due diligence in site selection, material palette selection, the type of construction, and anticipated performance outcomes in emergency evacuation scenarios. The institutionalized aged are extremely vulnerable in light of the myriad life-threatening threats posed by climate change. 1a; 6c; 9a; 9b; 9d; 9e; 9i; 9j

References:
9g-1. Associated Press (2007) Katrina flooding ‘unimaginable’: Official at nursing home deaths trial, CBCNews/World, 17 August. *
9g-2. Engberg, J. B. , & Castle, N. (2008). Health outcomes of nursing home residents following post-Katrina relocation. The Gerontologist, 33(6), 661-687. (PDF)
9g-3. Robinson, Kelly (2013) Eight years after Katrina: St. Rita’s owners still feel the stigma, ABC News, 29 August. *
Verderber, S. (2016). Innovations in Transportable Healthcare Architecture. London: Routledge.*
9h. Ecohumanism and Cost Containment
Ecologically and humanely sustainable –ecohumanist—LTC homes exhibit an equal prioritization on both human and ecological resources and associated affordances. Ten territories for engagement were recently delineated by Peters and Verderber (2017): (1) Minimization of the facility/campus carbon footprint; (2) Resilient and regenerative care settings; (3) The use of functional deconstruction strategies to reduce the sheer scale of institutions; (4) The role of landscape therapeutics and nature in treatment and healing; (5) The role of residentialism versus the anachronistic traditions of sheer institutionalism and custodialism; (6) An emphasis on stakeholder advocacy and social inclusiveness; (7) The value of therapeutic interior realms; (8) Incorporation of tectonic innovation; (9) The creative repurposing of existing resources to new uses versus thoughtless demolition; and (10) The importance of interdisciplinary knowledge mobilization. Building Information Modeling (BIM) in healthcare facility planning and design, combined with a controlled—versus controlling—use of LEAN in building design/delivery procurement can be cost effective if carefully balanced.
The value engineering of building materials with the aim of eliminating waste can reduce project delivery cost and improve timeline efficiencies; this allows for the reduction of total energy expenditures. The assumption is that an ecologically self-sufficient LTC home and its exterior environs will tread far less on the earth. BIM provides for monitoring occupants’ daily energy consumption, waste management practices, and can generate code compliance data for application in new and in renovated LTC facilities. Additional applications include geothermal system modeling, the comparative rating of carbon neutral materials and building assemblies, offsite prefabrication options for components, LED lighting and natural ventilation systems, roof rainwater harvesting, green roofs, and site landscaping options, including xeriscaping. The International Facility Management Association (IFMA) has a focus group area that addresses these and numerous other design attributes for application in the ecohumanist planning, design, construction, and daily management of LTC residential environments. 4e; 4h; 6d; 8a; 8b; 9a; 9c; 9e; 9i; 9j

References:
9h-1. Grunden, N., & Hagood, C. (2012) Lean-Led Hospital Design: Creating the Efficient Hospital of the Future, Boca Raton: CRC Press/Taylor & Francis.*
9h-2. International Facilities Management Association (2017) Operations and Maintenance Benchmarks Survey for Healthcare Facilities. IFMA.*
9h-3. Peters, T. & Verderber, S. (2017). Territories of engagement in the design of ecohumanist healthcare environments, Health Environments Research & Design Journal, 10(2), 104-123. (PDF)
9i. Participatory Design Strategies—Covid-19 and Beyond
The forced relocation of nursing home residents began en masse in the 1960s. The first wave occurred when increasing bed-space pressures in hospitals in Ontario and elsewhere resulted in pressures to convert the Geriatric Inpatient Ward into a Medical-Surgical Unit, and to related inpatient support functions. The need had arisen for the construction of hundreds of freestanding nursing institutions on the premise the “patient” would be far better served if housed in a completely separate institutional setting dedicated to one’s unique medical needs. Geriatric patients were moved out of hospitals and into “nursing homes” often designed in the minimalist International Style. Soon, patients were being forcibly transferred from older to newer nursing care institutions. The competitive push for modernization and the rise of suburbia were two of many underlying factors. The forced relocation of the aged resulted in alarmingly high mortality rates. By the late 1970s, published research studies had documented this. Lack of freedom of choice on the part of the family and the patient were cited, combined with the absence of pre and post-move orientation.
In the 1960s the participatory design movement emerged. It manifested in the mission of the Environmental Design Research Association (EDRA), founded in 1968. The earliest post-occupancy evaluations of recently-built nursing homes first appeared at this time. While considered an improvement over the old geriatric hospital wards these new quarters were found lacking in quality of life amenities and home-like aesthetics. These shortcomings were attributed to top-down institutional polices that failed to be inclusive—the family and the patient were rarely consulted regarding design options with respect to the planning and design of a new facility. This inattention to user-occupant needs and aspirations became the subject of many research studies focused on the aged and how they fared over time in the new generation of modernist LTC institutions. This is a concern that persists today—because the Covid-19 pandemic has placed a glaring spotlight on the plight of the residents and staff who inhabit and work in LTC homes. Participatory design methods–Co-Design—research knowledge is needed in professional practice to make LTC homes medically safer and more residential in every way possible. 6a; 9b; 9c; 9d; 9f; 9j
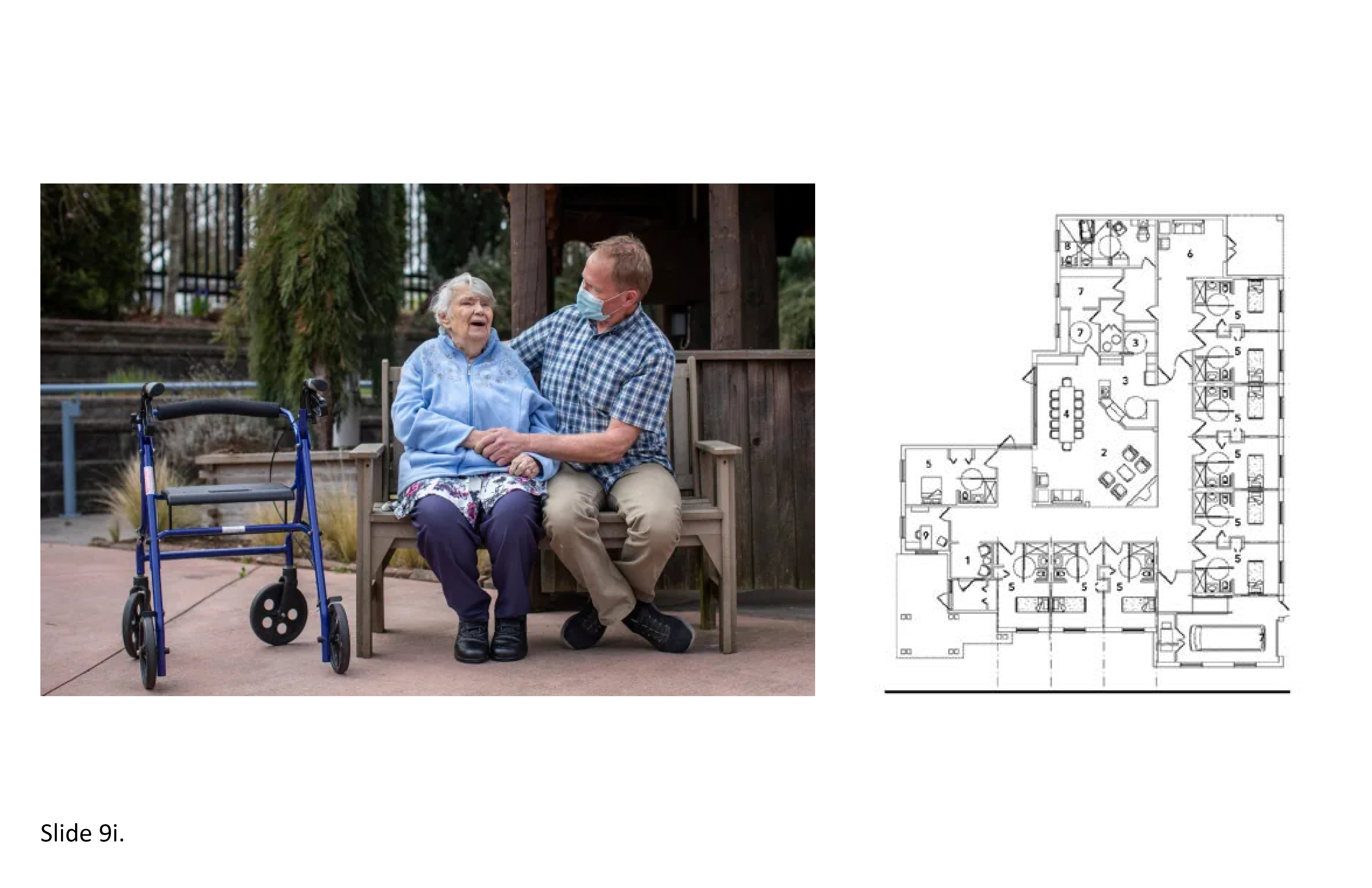
References:
9i-1. Cutler, L.J., & Kane, R.A. (2009). Post-occupancy evaluation of a transformed nursing home: The first four Green House settings. Journal of Housing for the Elderly, 23(4), 304-334. (PDF)
9i-2. Dixon, B, McHattie, S.M. & Broadley, C. (2022). The imagination and public participation: A Deweyan perspective on the potential of design innovation and participatory design in policy-making. Co-Design: International Journal of Co-Creation in Design and the Arts. 18(1): 151-163. (PDF)
9i-3. Elizarova, O & Dowd, K. (2017). Participatory design in practice. UX Magazine. 14 December. (PDF)
9i-4. Kelsey, S., Laditka, S., & Laditka, J. (2009). Dementia and transitioning from assisted living to memory care units: Perspectives of administrators in three facility types. The Gerontologist, 50(2), 192–203. (PDF)
9i-5. Zhu, X., Lee, H., Sang, H., Muller, J., Yang, H., Lee, C., & Ory, M. (2022). Nursing home design and COVID-19: Implications of guidelines and regulation. Journal of the American Medical Directors Association. (PDF)
9j. Salutogenic Design and Facility Procurement
Salutogenic design and Public–Private Partnerships (PPPs) may at first seem to be incompatible with one another. The former focuses on health promotion, improving the quality of life through design excellence, and life-affirming aspects of built and natural environments. The latter is premised mainly on a set of business procedures to ensure the highest return on investment. Innovative strategies must be in place in order to achieve success in synthesizing these seemingly disparate worlds. The ‘pros’ of PPPs include direct lines to private capital markets, the ability to integrate total building delivery from project start to facility commissioning, the imposition of strict protocols during the land and facility procurement process with the aim of achieving on-time and on-budget building delivery. PPPs aim to spread out the investment risk over many years relative to the initial financial investment. They establish long-term contractual relationships for building delivery and maintenance over up to a 30-year timeframe, and allow projects to be built that otherwise might not have been built. Oft-cited ‘cons’ of PPPs include a procurement process that is tediously slow to set up and get approved by all participating oversight agencies, and the likelihood of multiple legal disputes arising between a complex web of participants that can harm the design quality of the built outcome.
Classic PPPs often incur higher up-front borrowing costs with concomitant pressures to maximize shareholder financial return. The pressure is then on to build as cheaply as possible. What incentive is there to exceed minimum design quality standards? Worse, promises made upfront during a project’s bidding phase can end up being ignored when the winning bidder takes over, and the entire endeavor sours. PPPs are by design teams of rival individuals, firms, and corporations. Finally, overzealousness on the front end can diminish the final outcome. Salutogenic design concepts have been sidetracked because of LEAN. Many seasoned architects in the Province of Ontario maintain the current LTC facility procurement process is flawed and in need of an overhaul. One answer: Provide the public with the choice to decide where they will live. Put the power in the consumer’s hands. Create municipal/private sector partnerships where the land is provided up front by the local government. This can make available more “downtown” sites that are far better connected versus remote edge-of-town sites. 1a; 1c; 4a; 4c; 4f; 4g; 5c; 9c; 9d; 9e; 9h; 9i
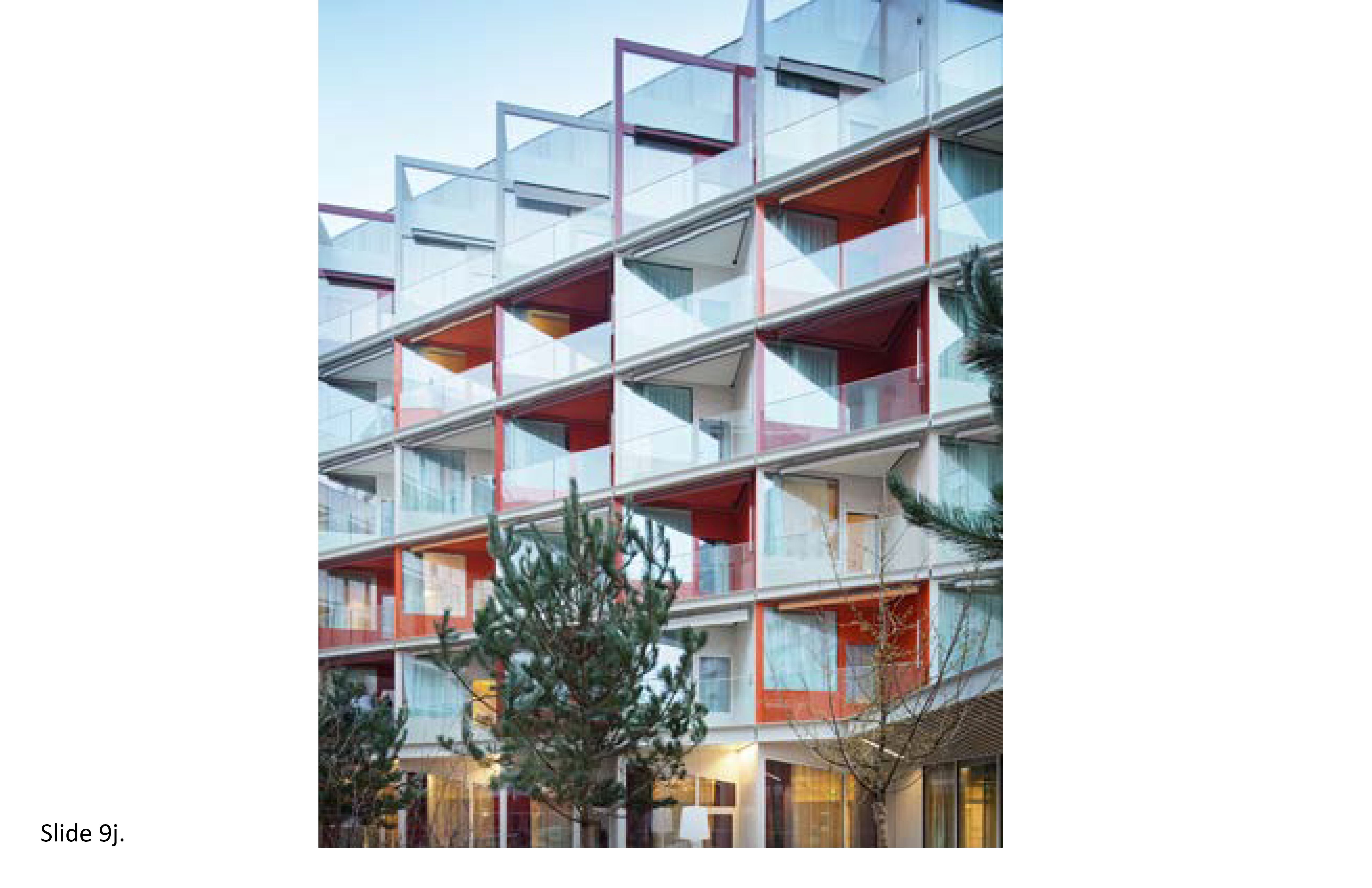
References:
9j-1. Clark, M. et al. (2016). Innovative public-private partnerships to enhance aging in place in the United States,’ Human Research Center Research Report #26. New Brunswick, NJ: Rutgers School of Social Work. (PDF)
9j-2. Craig, C. (2017). Imagined futures: Designing future environments for the care of older people. The Design Journal, 20(1), S2336–S2347. (PDF)
9j-3. Hodgson, Nancy A. (2020) Aging in Place: The Role of Public-Private Partnerships. Wharton Pension Research Council Working Papers. 691. (PDF)
9j-4. International Facilities Management Association (2017) Operations and Maintenance Benchmarks Survey for Healthcare Facilities. IFMA. Online.*
9j-5. McFadden, E.S., & Lucio, J. (2014). Aging in (privatized) places: Subsidized housing policy and seniors. Journal of Housing for the Elderly, 28(3), 268–287. (PDF)
9j-6. Schwarz, Ken (2015) Can salutogenic outcomes be achieved through public private partnerships? World Health Design, 8(6): 68-77. *